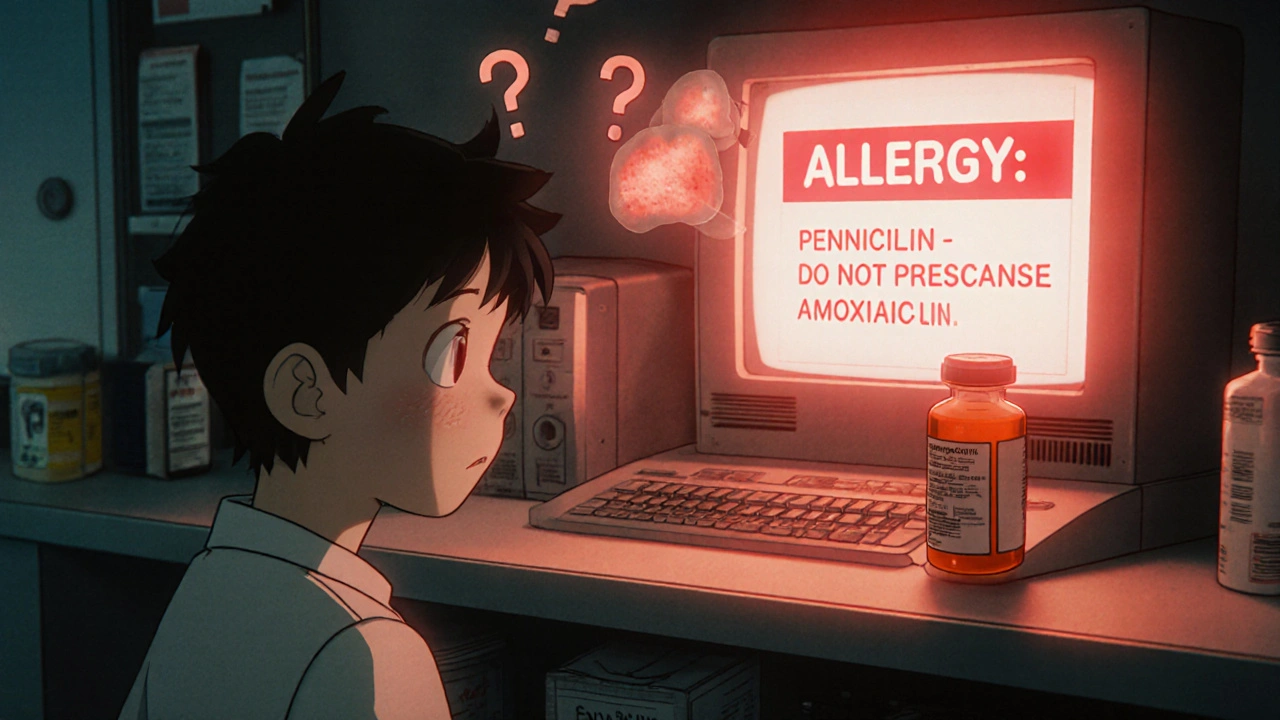
When you pick up a prescription, you might see a red or yellow pop-up on the pharmacy screen saying, "Allergy: Penicillin. Do not dispense Amoxicillin." It feels serious. But here’s the truth: most of these alerts are wrong. You’re not alone if you’ve seen one and thought, "Wait, I took that before and I’m fine." That’s not a glitch-it’s the system working exactly as designed, just not well.
What Pharmacy Allergy Alerts Actually Are
Pharmacy allergy alerts are automated warnings built into electronic health record (EHR) systems like Epic, Cerner, and Allscripts. They pop up when a doctor prescribes or a pharmacist fills a medication that might conflict with a patient’s documented allergy. These systems use databases like First DataBank to cross-check drugs against allergy lists. They don’t guess-they follow rules. But those rules are outdated, overly broad, and often trigger false alarms.The Two Types of Alerts (And Why It Matters)
There are two kinds of allergy alerts you’ll see:- Definite allergy alerts: The system sees an exact match. Patient documented penicillin allergy? Prescribing penicillin? Alert triggers. This one is usually correct.
- Possible allergy alerts: The system sees a class match. Patient has penicillin allergy? Prescribing cephalexin (a cephalosporin)? Alert triggers-even though the actual risk of cross-reaction is less than 2%.
Here’s the kicker: 90% of all allergy alerts are possible alerts. That means most of the time, the system isn’t warning you about a confirmed danger-it’s warning you about a theoretical one based on outdated science.
Why So Many Alerts Are Wrong
The biggest problem? Poor documentation. Patients often say, "I had a rash after penicillin," and the system records it as "Penicillin allergy" without context. But rashes aren’t always allergies. Many are side effects-like nausea from metformin or a headache from aspirin. These aren’t immune reactions. They’re not allergies at all.Another issue: cross-reactivity myths. For decades, doctors were taught that if you’re allergic to penicillin, you can’t take cephalosporins. That’s not true anymore. Modern research shows the real cross-reactivity rate is under 2% for later-generation cephalosporins like cefdinir or ceftriaxone. Yet 89% of EHR systems still flag them as high-risk.
Even worse, some systems treat every reaction the same. A mild rash from a childhood dose of amoxicillin? Same alert level as anaphylaxis. That’s why clinicians override them. In a 2020 study, over 75% of life-threatening allergy alerts were overridden because they were false.
How to Read the Alert Correctly
When an alert pops up, don’t just click "Continue." Ask yourself these four questions:- What’s the documented reaction? Was it a rash? Hives? Swelling? Trouble breathing? Nausea? Only hives, swelling, or anaphylaxis are true IgE-mediated allergies. Nausea, diarrhea, or headaches? That’s an adverse reaction-not an allergy.
- When did it happen? True allergic reactions usually show up within minutes to two hours after taking the drug. A rash that appeared three days later? Likely not immune-mediated.
- Is this a class alert? Is the system warning you about a whole drug family? Penicillin → cephalosporin? NSAID → all NSAIDs? These are the most likely to be false. Check the specific drug, not the group.
- Have you taken this before? If you’ve taken amoxicillin five times without issue, that’s more evidence than a 20-year-old note in your chart.
Pharmacists and doctors need to treat these alerts like clues-not commands. The alert is a starting point for conversation, not a reason to skip a needed medication.
The Overriding Problem
Clinicians override these alerts more than 95% of the time. That’s not negligence-it’s survival. If you get 17 alerts for one prescription because a patient once had a stomachache after penicillin, you stop paying attention. That’s called alert fatigue. And it’s dangerous.A 2022 study found that 78% of physicians override allergy alerts several times a week. On Reddit, doctors shared stories like: "I got 12 alerts for vancomycin because a 5-year-old patient had a fever after amoxicillin." That’s not a warning. That’s noise.
But here’s the real risk: when the system stops being trusted, even the true alerts get ignored. If a patient has a real anaphylactic history and the system flags a related drug, but the clinician has been conditioned to click through, they might miss it.

What’s Changing? Better Systems Are Coming
The industry knows the problem. New updates are starting to fix it:- Reaction-specific documentation: Systems now ask for details: "What happened? When? How severe?" Mayo Clinic saw accurate allergy records jump from 39% to 76% after requiring this.
- Machine learning scoring: Epic’s 2023 update uses AI to predict which alerts are likely to be false based on past override patterns. At Intermountain Healthcare, low-value alerts dropped by 37%.
- Integration with allergy testing: If a patient had a drug challenge test (where they’re safely re-exposed to confirm or rule out allergy), that result now auto-updates the alert system. Oracle Health’s new "Precision Allergy" module does this.
- Risk-stratified alerts: Instead of one red flag for everything, systems now use color tiers: yellow for mild, red for life-threatening. Only severe reactions trigger mandatory stops.
By 2026, 70% of major EHR systems are expected to use these smarter methods. That means fewer alerts-but more accurate ones.
What You Should Do
If you’re a patient:- Don’t assume your allergy list is correct. Review it at every visit.
- If you’ve taken a drug before without issue, say so. "I took amoxicillin last year and felt fine." That’s more valuable than a note from 15 years ago.
- Ask: "Was this reaction really an allergy, or just a side effect?"
If you’re a provider:
- Don’t override blindly. Use the alert to ask questions, not avoid them.
- Update documentation after every encounter. Replace "penicillin allergy" with "rash after amoxicillin at age 7, no reaction since."
- Refer patients for allergy testing if they have a vague history. Penicillin allergies are often overdiagnosed-and can be safely removed.
The Bottom Line
Pharmacy allergy alerts are meant to save lives. But right now, they’re drowning us in false alarms. The system isn’t broken-it’s just badly programmed. The real solution isn’t more alerts. It’s better data. Clearer documentation. Smarter rules.The next time you see an alert, pause. Ask what it’s really telling you. Because the difference between a life saved and a life harmed isn’t always in the drug-it’s in the detail behind the warning.
Are all drug allergy alerts accurate?
No. Around 90% of pharmacy allergy alerts are triggered by cross-reactivity concerns or vague reaction histories-not confirmed allergies. Studies show that only 12% of NSAID alerts and less than 2% of penicillin-cephalosporin alerts represent real risks. Most are false positives caused by outdated documentation or broad class-based rules.
What’s the difference between an allergy and an adverse reaction?
An allergy involves the immune system reacting to a drug, often causing hives, swelling, trouble breathing, or anaphylaxis. An adverse reaction is a side effect-like nausea, dizziness, or headache-that doesn’t involve the immune system. Only immune-mediated reactions are true allergies. Many patients label side effects as allergies, which leads to misleading alerts.
Can I outgrow a drug allergy?
Yes. Up to 80% of people who report a penicillin allergy in childhood lose it over time, even without testing. If you had a rash as a kid but have taken penicillin since without issue, you likely aren’t allergic anymore. Formal allergy testing can confirm this and remove the alert from your record.
Why do I get alerts for drugs I’ve taken before?
Because your allergy list hasn’t been updated. If you had a mild reaction years ago and later took the same drug without issue, the system doesn’t know that unless you or your provider updated the documentation. EHRs don’t auto-correct-they store what’s entered. Always review your allergy list at every visit.
Should I avoid a drug just because of an alert?
Not automatically. If the alert is for a drug you’ve safely taken before, or if the reaction was mild (like a rash or stomach upset), discuss it with your provider. Many alerts are based on outdated or incorrect info. The alert is a flag for review, not a rule to never use the drug. Never ignore it-but don’t assume it’s a hard stop either.






Karen Willie
November 22, 2025 AT 22:54It’s wild how we treat these alerts like gospel when they’re basically digital noise. I had a rash from amoxicillin at 8, and for years I was told I couldn’t take any penicillin-class drugs. Then I got pneumonia and my doctor said, ‘Let’s just try it.’ I’m fine. No reaction. Turns out, I never had an allergy-just a weird skin thing. These systems need to stop treating every childhood rash like a death sentence.
Archana Jha
November 24, 2025 AT 13:24lol so the pharma companies and big tech are in cahoots?? epic and cerner dont wanna fix this because if people stop getting allergic alerts then they’ll have to sell MORE drugs to replace the ones we’re ‘forbidden’ from taking. also, did you know the FDA gets funding from drug makers? coincidence? i think not. the ‘allergy’ thing is just a distraction so we keep buying meds we dont need. wake up sheeple.
Aki Jones
November 26, 2025 AT 12:14Let’s be clear: this isn’t a ‘system design flaw’-it’s a systemic failure of accountability. EHR vendors prioritize speed over safety, and clinicians, conditioned by alert fatigue, have abdicated clinical judgment to algorithmic convenience. The 90% false-positive rate isn’t an accident-it’s the inevitable outcome of commodified healthcare infrastructure. We’ve outsourced critical thinking to a vendor’s API, and now we’re surprised when it fails catastrophically. This isn’t just bad UX-it’s a public health liability.
prasad gaude
November 26, 2025 AT 18:15In India, we don’t even have proper EHRs in most clinics. But when we do, the same thing happens-someone writes ‘allergy to medicine’ and everyone panics. My uncle got a rash from a cough syrup in 1995, and now no doctor in town will give him any painkiller. They don’t ask questions. They just say ‘no.’ It’s funny how technology, meant to help, ends up making things more rigid. Maybe we need less tech and more human conversation.
Timothy Sadleir
November 27, 2025 AT 00:53While I appreciate the sentiment expressed in this article, I must emphasize that the fundamental issue lies not in the software, but in the erosion of professional standards. The fact that clinicians override alerts 95% of the time speaks volumes about the decline in clinical diligence. The system is not broken-it is being misused. If physicians would take the time to properly document and verify allergies, rather than reflexively clicking through, these alerts would serve their intended purpose. This is not a technological problem; it is a cultural one.
Jennifer Griffith
November 27, 2025 AT 02:54so like… i had a rash from amoxi like 10 yrs ago and now i get 5 alerts every time i need antibiotics? smh. i just tell the pharmacist i’m fine and they shrug. why cant the system just remember when i took it before and didn’t die??
Roscoe Howard
November 28, 2025 AT 14:32Let me be blunt: this is yet another example of how American healthcare has been corrupted by corporate interests. EHRs are designed by contractors who have never held a stethoscope. They prioritize liability over logic, and the result is a system that terrifies patients and exhausts providers. The fact that we tolerate this is a national disgrace. We need a federal mandate to overhaul these systems-not patches, not ‘updates,’ but a full reset. Anything less is complicity.
Patricia McElhinney
November 29, 2025 AT 14:36Anyone who says ‘I’ve taken it before so it’s fine’ is dangerously naive. Allergies can develop at any time. Just because you survived it once doesn’t mean you won’t die next time. The system isn’t perfect-but it’s the only thing standing between you and anaphylaxis. You don’t get to decide what’s ‘real’ based on anecdote. That’s how people die. Stop being so casual about life-or-death medical data.
Agastya Shukla
November 30, 2025 AT 15:04Interesting. I’ve worked with EHR systems in rural clinics, and the biggest hurdle isn’t the tech-it’s the patient’s own understanding. Many don’t know the difference between a rash and anaphylaxis. They say ‘allergic’ because they were told to. The real fix? Medical literacy. Train patients to describe reactions accurately, and the alerts become useful again. Not magic AI. Just better communication.