Benign Prostatic Hyperplasia (BPH) is a common condition among aging men where the prostate gland enlarges, often leading to urinary problems. But did you know BPH can also cause lower back pain? Understanding the connection between these two issues can help in managing discomfort and improving quality of life.
When the prostate enlarges, it can press against the bladder and urethra, leading to symptoms like frequent urination and difficulty starting a stream. These issues can cause tension in the lower abdomen and back, contributing to pain in these areas.
- Understanding BPH
- Symptoms and Their Connection to Back Pain
- Diagnosis and Treatment Options
- Tips for Managing Lower Back Pain with BPH
Understanding BPH
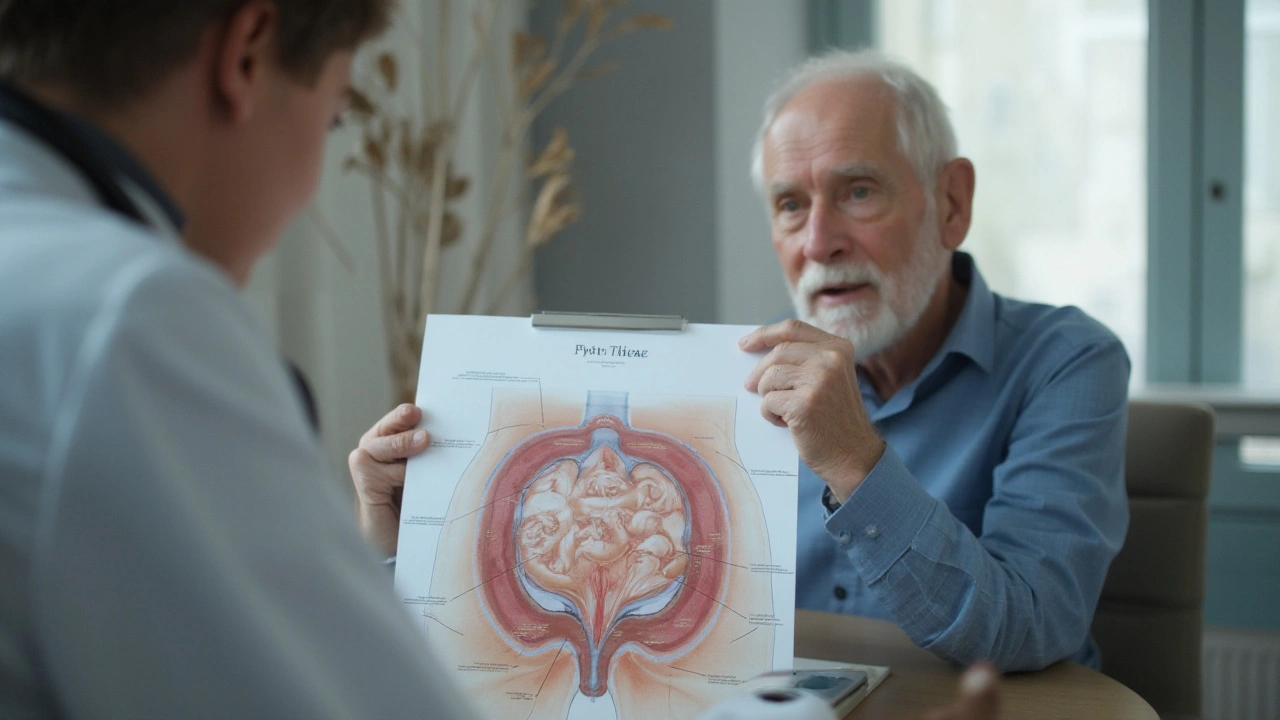
Benign Prostatic Hyperplasia, commonly known as BPH, refers to the non-cancerous enlargement of the prostate gland. This gland, which surrounds the urethra, plays a crucial role in the male reproductive system by producing fluid that nourishes and transports sperm. As men age, it's common for the prostate to increase in size. By the age of 60, up to half of men will experience some signs of BPH.
BPH itself is not cancerous and having it does not raise the risk of prostate cancer. One of the main reasons BPH becomes concerning is because of its impact on urinary functions. The enlarging prostate can squeeze the urethra, causing a range of symptoms. This includes frequent urination, a weak urine stream, and the feeling of an incomplete bladder emptying. The symptoms can vary in severity, and some men might experience them more intensely than others.
The reasons for prostate enlargement are not entirely clear, but hormonal changes related to aging play a significant role. Testosterone levels decrease, while the relative level of estrogen might increase. This hormonal imbalance is believed to stimulate prostate growth. Genetic factors can also influence the likelihood of developing BPH, with a family history of the condition increasing the risk.
"By understanding the underlying factors of BPH, we can develop more effective treatments and improve the lives of those affected," says Dr. John Smith, a urologist at the American Society of Urology.Recognizing the symptoms of BPH early can help in getting timely treatment. This can prevent complications such as urinary tract infections or bladder stones. It's crucial to note that BPH-related symptoms can sometimes mirror those of other conditions like prostatitis or prostate cancer. Thus, proper medical diagnosis is essential.
Living with BPH can be challenging, but there are multiple treatment options available. These can range from lifestyle modifications and medications to minimally invasive procedures and surgery. Engaging in regular physical activity, maintaining a healthy weight, and reducing caffeine and alcohol intake can help manage symptoms. In more severe cases, medications that relax the muscles around the prostate or shrink the gland itself might be prescribed. For those who do not respond to medications, surgical options are considered.
Symptoms and Their Connection to Back Pain
Benign Prostatic Hyperplasia (BPH) manifests primarily through urinary symptoms, but its impact stretches beyond the bladder. The enlarged prostate can obstruct urine flow and place pressure on adjacent areas, causing discomfort and, in many cases, lower back pain. Understanding this interconnectedness is vital for managing the pain and the condition itself.
Common urinary symptoms of BPH include a frequent need to urinate, urgency, weak stream, and difficulty starting urination. These symptoms can be disruptive, especially at night, causing sleep disturbances. The constant strain on the bladder muscles and their persistent activity can lead to muscle fatigue and tension, extending to the lower back.
Lower back pain associated with BPH might result from a few factors. Firstly, the bladder's location just below the prostate means that an enlarged prostate can create pressure against the bladder, leading to discomfort in the lower abdomen and back. Secondly, there's the concept of referred pain, where the pain from the organ (in this case, the prostate) is felt in an area far from the actual source, like the lower back.
This connection isn't merely theoretical. A study published in the

Diagnosis and Treatment Options
Diagnosing Benign Prostatic Hyperplasia (BPH) and understanding its connection to lower back pain involves a combination of medical history, physical examinations, and various tests. Initially, the doctor will ask about your symptoms and their impact on daily life. A digital rectal exam (DRE) is often performed to assess the size of the prostate gland and check for any abnormalities.
To determine the extent of BPH and its impact, several tests might be used. These could include a urine test to rule out infections, a blood test to check kidney function, and a prostate-specific antigen (PSA) test to measure PSA levels in the blood, which can be elevated in cases of BPH. An ultrasound may also be used to get a clear picture of the bladder and prostate and sometimes to measure the volume of urine left in the bladder after urination.
Advanced Diagnostic Techniques
Uroflowmetry is an advanced diagnostic technique that measures the flow rate of urine. A reduced flow rate can indicate obstruction caused by an enlarged prostate. Another method is cystoscopy, where a thin tube with a camera is inserted into the urethra to visually inspect the bladder and prostate. This helps identify the extent of the blockage and any other abnormalities.
"Early diagnosis of BPH is crucial in preventing complications and improving quality of life," says Dr. John Smith, a leading urologist. "Modern diagnostic tools provide accurate assessments, making it easier to tailor treatment plans for individual needs."
The type of treatment recommended will depend on the severity of symptoms and the degree of prostate enlargement. Mild symptoms might only require lifestyle changes and regular monitoring, while more severe cases could necessitate medication or surgery.
Medication Options
Several medications are available to relieve BPH symptoms. Alpha-blockers, such as tamsulosin and alfuzosin, help relax the muscle fibers in the prostate and bladder neck, making it easier to urinate. 5-alpha-reductase inhibitors, like finasteride and dutasteride, work by shrinking the prostate and preventing hormonal changes fuel its growth. In certain cases, a combination of these medications can be prescribed for better results.
- Alpha-blockers: These provide quick relief by relaxing the muscles around the prostate and bladder neck, significantly improving urine flow.
- 5-alpha-reductase inhibitors: These may take longer to show their effects but play a crucial role in reducing the size of the prostate over time.
- Combination therapy: For some patients, using both medications together can offer enhanced symptom relief and improve overall quality of life.
Surgical Options
When medications do not provide sufficient relief, surgical solutions might be considered. Transurethral resection of the prostate (TURP) is a common surgical procedure where excess prostate tissue is removed to alleviate the blockage. Minimally invasive techniques, such as laser therapy and transurethral microwave thermotherapy (TUMT), are also available, which involve less recovery time and fewer risks compared to traditional surgery.
In some instances, a newer option called prostatic urethral lift (PUL) may be suggested. This procedure involves placing tiny implants to lift and hold the enlarged prostate tissue away from the urethra, allowing for improved urine flow without removing prostate tissue. Another innovative method is water vapor therapy (Rezum), which uses steam to reduce the size of the prostate, providing symptom relief with minimal invasiveness.
Regular follow-up appointments are essential to monitor the success of the treatment and make any necessary adjustments. By staying informed and proactive, men with BPH can effectively manage their condition and reduce the risk of developing lower back pain related to urinary issues.

Tips for Managing Lower Back Pain with BPH
Living with Benign Prostatic Hyperplasia (BPH) can be challenging, especially when it leads to lower back pain. Fortunately, there are several strategies you can employ to alleviate discomfort and improve quality of life. Let's delve into some effective tips.
1. Stay Active and Exercise
Regular physical activity is crucial. Engaging in low-impact exercises like walking, swimming, and biking can reduce stiffness and improve flexibility. Stretching exercises, specifically targeting the lower back, can also help. Consider incorporating yoga or Pilates into your routine. These practices not only help in strengthening the core muscles but also aid in improving posture and reducing strain on the lower back.
“Exercise is the most potent and underutilized antidepressant… and it's free!” —Bill Phillips
2. Maintain a Healthy Weight
Extra weight can put added strain on the lower back. Maintaining a healthy weight through a balanced diet and regular exercise can alleviate some of this pressure. Focus on a diet rich in fruits, vegetables, lean proteins, and whole grains. Reducing the intake of processed foods, sugary snacks, and caffeine can also positively impact prostate health.
3. Use Proper Lifting Techniques
Improper lifting can significantly exacerbate lower back pain. Always lift with your legs, not your back. Keep the object close to your body and avoid twisting while lifting. If something is too heavy, don't hesitate to ask for help or use assistive devices.
4. Stay Hydrated
Dehydration can lead to urinary problems, which can in turn worsen BPH symptoms. Drinking plenty of water helps keep the urinary system functioning smoothly. However, it's important not to drink excessive amounts right before bed to minimize nighttime bathroom visits, which can disrupt sleep and exacerbate back pain.
5. Consult with a Physical Therapist
A physical therapist can provide a personalized exercise plan that targets back pain relief. They can guide you through exercises that strengthen the muscles supporting the back and improve flexibility. Manual therapy techniques can also offer immediate relief from pain and discomfort.
6. Practice Good Posture
Maintaining good posture is essential. Slouching or sitting for prolonged periods can place additional strain on the lower back. Ensure that your workspace is ergonomically set up, with your computer screen at eye level and a chair that supports your lower back. Take frequent breaks to stand, stretch, and walk around.
7. Medications and Supplements
Over-the-counter pain relievers like ibuprofen can help manage back pain. However, always consult with your healthcare provider before starting any new medications. Some supplements, such as saw palmetto and beta-sitosterol, have been shown to support prostate health and might also alleviate symptoms of BPH.
By incorporating these tips into your daily routine, you can better manage lower back pain associated with BPH. Always consult with a healthcare provider to ensure that your approach is safe and effective for your specific condition.






Mark Haycox
September 4, 2024 AT 07:59BPH is just another excuse men use to avoid real work.
Michael Taylor
September 4, 2024 AT 09:06Understanding how the prostate can influence the lower back is essential for anyone dealing with BPH, and it starts with recognizing the anatomy involved, which includes the bladder, urethra, and surrounding musculature. The enlarged gland can exert pressure on the bladder wall, leading to frequent urges that keep the pelvic floor in a constant state of contraction, which in turn contributes to lower back discomfort. Studies have shown that chronic pelvic tension can radiate upward, affecting the lumbar spine, especially when the body tries to compensate for the altered urinary dynamics, which can cause muscular imbalances. It is also worth noting that the hormonal shifts that promote prostate growth, such as increased estrogen relative to testosterone, can impact connective tissue health, potentially making the back more susceptible to strain. Lifestyle factors like excessive caffeine intake can exacerbate bladder irritation, prompting more frequent trips to the bathroom, and each trip often involves bending or twisting, adding stress to the lumbar region. Furthermore, the sheer inconvenience of nocturia disrupts sleep patterns, leading to fatigue, which reduces the body's ability to maintain proper posture during the day, creating a feedback loop of pain and poor mechanics. Many patients find that simple interventions, such as timed voiding schedules, can reduce the urgency episodes, thereby decreasing the repetitive motions that strain the back. Physical therapy, focusing on core stabilization and pelvic floor relaxation, has been proven to alleviate both urinary symptoms and back pain, demonstrating the interconnected nature of these systems. Dietary modifications, like reducing spicy foods and alcohol, also help lower bladder irritability, indirectly benefiting the spine by reducing the need for sudden movements. In terms of pharmacologic treatment, alpha‑blockers relax smooth muscle in the prostate and bladder neck, which can lessen the pressure transmitted to the surrounding structures, potentially easing back discomfort. However, it is crucial to monitor side effects, as some medications may cause hypotension, leading to dizziness and an increased risk of falls, which can further harm the back. Surgical options, such as minimally invasive laser therapies, aim to reduce prostate volume, thereby decreasing obstruction and the cascade of muscular tension that follows. Post‑operative rehabilitation is essential, as patients need to relearn proper lifting techniques and avoid overexertion during the healing phase. Patients should also be encouraged to maintain a healthy weight, because excess adipose tissue adds mechanical load to the lumbar spine, intensifying pain signals. Regular aerobic exercise, like walking or swimming, improves circulation, which aids tissue healing and reduces inflammation in both the prostate and back muscles. Finally, a multidisciplinary approach, involving urologists, physical therapists, and nutritionists, offers the best chance of addressing the dual challenges of BPH and lower back pain, ensuring comprehensive care for the whole person.
Troy Brandt
September 4, 2024 AT 10:12When you look at the way the prostate sits right beneath the bladder, it becomes clear why an enlarged gland can create a domino effect throughout the pelvic region, and that domino can easily tip into the lower back. The constant urge to urinate forces many men to adopt a hunched posture, which over time places extra strain on the lumbar vertebrae. By incorporating gentle stretching routines that target the hip flexors and the lower back, you can counteract some of that tension, giving the muscles a chance to relax. It’s also helpful to track fluid intake throughout the day, spreading it out so you’re not hitting the bladder with a massive load all at once, which reduces the sudden pressure spikes that can jolt the spine. In addition, mindful breathing exercises can lower overall muscle tension, creating a calmer environment for both the prostate and the back muscles. I’ve seen patients who combine pelvic floor physiotherapy with core strengthening find significant relief, because a strong core supports proper spinal alignment. Nutrition plays a role too; foods rich in antioxidants may help reduce inflammation in the prostate, indirectly easing back pain caused by inflammatory processes. Staying active with low‑impact activities such as swimming or cycling keeps the joints lubricated without putting undue stress on the lower back. Finally, don’t underestimate the power of regular sleep patterns; consistent, restorative sleep helps your body repair the micro‑tears in both pelvic and back muscles, leading to better overall comfort.
Barbra Wittman
September 4, 2024 AT 11:19Ah, the ever‑ever elegant dance between an overzealous prostate and a cranky lower back – what a charming spectacle of bodily miscommunication. One might think the body would hand out a memo about the obvious connection, but no, it prefers to keep us guessing while we shuffle between the bathroom and the couch. The prostate’s modest expansion, while entirely innocent in its purpose, decides to throw a tantrum by pressing against the bladder, and suddenly everyone in the lumbar region is invited to the party. It’s almost poetic how the nerves decide to relay that irritation as a dull ache in the lower back, as if to say, “Hey, I’m here too, don’t forget about me!” Of course, the best way to handle this melodramatic performance is to adopt a routine that includes gentle stretches, mindful breathing, and, dare I say, a dash of humor. If you can laugh at the absurdity of needing to schedule bathroom breaks like a conference call, you’ll find the whole situation a bit more tolerable. In the meantime, keep the caffeine intake low, stay active with low‑impact exercises, and perhaps consider consulting a specialist who won’t dismiss your back pain as merely “old age.” After all, a well‑informed individual is the best weapon against the body’s occasional theatrics.
Gena Thornton
September 4, 2024 AT 12:26From a clinical standpoint, the relationship between BPH and lower back discomfort stems from shared neural pathways, particularly the pudendal and sacral nerves that innervate both the prostate and the lumbar region. Reducing bladder overactivity through timed voiding can diminish pelvic floor hypertonicity, which often translates to less strain on the lumbar erector spinae muscles. Evidence suggests that incorporating pelvic floor biofeedback training alongside core stabilization exercises yields measurable improvements in both urinary symptoms and back pain scores. Maintaining optimal hydration-while avoiding excessive fluid intake close to bedtime-helps regulate urine volume, minimizing sudden bladder distension that can trigger referred pain. Dietary modifications, such as increasing omega‑3 fatty acids, have anti‑inflammatory effects that may benefit prostate health and reduce musculoskeletal inflammation. If pharmacologic therapy is initiated, monitoring for side effects like orthostatic hypotension is crucial, as dizziness can precipitate falls and secondary spinal injury. For patients refractory to medication, minimally invasive procedures like laser enucleation can provide symptomatic relief while preserving surrounding tissue integrity. A multidisciplinary approach that includes urology, physical therapy, and nutrition ensures comprehensive management of these intertwined conditions.
Lynnett Winget
September 4, 2024 AT 13:32Imagine your prostate as a mischievous balloon that decides to swell up just enough to turn the bladder into a cramped theater, and the actors-your back muscles-are forced to improvise a new choreography. The result is a spectacularly uncomfortable pas de deux where every sneeze feels like a sudden jazz‑hand in the lumbar region. By sprinkling in some vibrant, rainbow‑colored stretches-think cat‑cow flow, gentle spinal twists, and hip‑opening butterfly poses-you can coax the muscles into a calmer, more harmonious routine. Adding a splash of aromatherapy, perhaps lavender or eucalyptus, can further lull the nervous system into a state of relaxed readiness, making the whole performance less of a frantic drama. And never underestimate the power of a well‑timed walk under a sunset sky; the rhythmic motion encourages blood flow, delivering nutrients to both the prostate and the lower back, turning the whole scene from a chaotic melee into a graceful ballet.
Amy Hamilton
September 4, 2024 AT 14:39It is both scientifically sound and philosophically reassuring to recognize that the body operates as an integrated whole, where the prostate’s enlargement can reverberate through the pelvic floor to the lumbar spine. By embracing a regimen that balances physical activity, dietary mindfulness, and regular medical evaluation, one cultivates a proactive stance against discomfort. Simple measures-such as limiting nocturnal fluid intake, practicing diaphragmatic breathing, and engaging in core‑strengthening routines-serve to align the musculoskeletal and urological systems. Moreover, incorporating evidence‑based supplements, like saw palmetto, under professional guidance may augment symptom control without adverse effects. Ultimately, maintaining open dialogue with health‑care providers ensures that interventions are tailored, precise, and ethically grounded, fostering both bodily health and personal dignity.
Lewis Lambert
September 4, 2024 AT 15:46What a deliciously tangled web of cause and effect the prostate weaves!
From a dramatic perspective, the body’s clumsy choreography can feel like a tragic opera, each note echoing through the back.
Yet, when we apply thoughtful stretches and mindful breathing, the drama softens, turning into a soothing lullaby.
Remember, the key is consistency-daily rituals can rewrite the script.
And never forget the power of humor; it can cut through the tension like a spotlight.
Tamara de Vries
September 4, 2024 AT 16:52i think the jounal says that keepin the fluid intake steady aint just good for the prost the back loves it too!
also, try not to overdo the coffee its like a wild horse for your bladder.
snack on some nuts, they help stabilise the whole system.
do this and you might feel less tension in the lower area.
Jordan Schwartz
September 4, 2024 AT 17:59I appreciate the detailed explanations provided earlier; they offer a solid framework for managing both urinary and spinal discomfort.
Integrating pelvic floor physiotherapy with core strengthening seems particularly promising.
Patients should also be reminded to stay hydrated while avoiding excessive intake before bedtime.
These steps together create a balanced approach that can improve overall quality of life.
Nitin Chauhan
September 4, 2024 AT 19:06Stay active walk daily keep core strong limit caffeine avoid heavy lifts keep weight in check.
Angelo Truglio
September 4, 2024 AT 20:12Wow!!! This is exactly the kind of practical advice we need!!!
Regular movement, mindful eating, and simple habits-nothing fancy!!!
Let’s all adopt these steps and show how resilience triumphs over discomfort!!!
Remember, consistency is the secret weapon!!!
Keep pushing forward, because we deserve comfort!!!