Feeling like the room is spinning when you roll over in bed? Or feeling off-balance walking down a grocery aisle? You’re not alone. About one in three people over 65 deal with some kind of balance problem, and vertigo is the most common reason they see a doctor. But here’s the catch: most people think it’s just dizziness. It’s not. Vertigo is a specific kind of spinning sensation-like you’re on a merry-go-round you didn’t get on. And it’s usually coming from your inner ear.
What’s Really Going On in Your Inner Ear?
Your inner ear isn’t just for hearing. It’s your body’s built-in gyroscope. Inside each ear, there are three fluid-filled loops called semicircular canals. Tiny crystals, called otoconia, sit in a nearby sac. These crystals help your brain sense head position and movement. When they get loose and drift into the wrong canal-usually the one pointing down your neck-you get vertigo. That’s benign paroxysmal positional vertigo, or BPPV. It’s the #1 cause of vertigo, responsible for up to 30% of all dizziness cases and half of all cases in older adults.Why You Feel Like You’re Spinning
When you move your head-say, turning to look over your shoulder-the loose crystals shift with the fluid in the canal. Your brain gets confused. It thinks you’re spinning, even though you’re not. That’s why BPPV hits with quick head movements: rolling over, sitting up, looking up at a shelf. Each episode lasts seconds to a minute, but the fear of it coming back can make you avoid those movements entirely. And that’s where the real problem starts: you start moving less, your balance weakens, and you’re more likely to fall.Other Inner Ear Culprits
BPPV isn’t the only player. Vestibular neuritis happens when a virus inflames the nerve that connects your inner ear to your brain. You get sudden, intense spinning that lasts days, sometimes weeks, but no hearing loss. Then there’s Meniere’s disease. It’s rarer but more complex. You get vertigo that lasts 20 minutes to half a day, plus ringing in the ear, muffled hearing, and that weird feeling of pressure. It’s caused by too much fluid building up in the inner ear. And while it sounds like a one-off problem, it often comes back-sometimes daily, sometimes months apart.Is It Your Brain? (The 20% You Can’t Ignore)
About 20% of vertigo cases come from the brain-not the ear. This is where things get serious. If your vertigo comes with double vision, slurred speech, numbness, or trouble walking straight, it could be a stroke. That’s why doctors now use the HINTS exam: a quick test that checks eye movements and head control. Done within 48 hours of symptoms, it’s 97% accurate at spotting stroke-related vertigo. Most people don’t know this. They assume dizziness is always harmless. It’s not. If vertigo hits suddenly and doesn’t improve in a day or two, get checked. Don’t wait.
Medication Isn’t the Answer (Most of the Time)
You’ve probably heard of meclizine (Antivert) or promethazine. These drugs calm the spinning feeling. They work-for a few hours. But here’s the truth: they don’t fix the problem. They just mask it. And if you take them for more than 72 hours, your brain stops learning how to compensate. That means recovery takes longer. The Children’s Hospital of Philadelphia found that long-term use delays natural healing by 30-50%. So yes, a pill might help you get through the first night. But it won’t stop the next attack.Vestibular Therapy: The Real Fix
This is where things change. Vestibular rehabilitation therapy (VRT) isn’t a magic trick. It’s physical therapy for your balance system. Think of it like rehab after a knee injury-but for your inner ear and brain. The goal? Train your brain to rely on other senses-your eyes and your body’s sense of position-to make up for the faulty signal from your ear.How It Works
For BPPV, the Epley maneuver is the gold standard. It’s a series of head positions that gently guide the loose crystals back into the right spot. Done right, it works in 80-90% of cases after one or two tries. You can do it at home with a video guide, but most people need a therapist to make sure they’re doing it correctly. The first time? It might make you dizzy. The second? Less so. The third? Usually gone.For Other Causes
If it’s vestibular neuritis or Meniere’s, VRT uses different exercises. Gaze stabilization helps you keep your eyes locked on a target while moving your head. Balance retraining teaches you to stand and walk safely on uneven surfaces. Habituation exercises slowly expose you to movements that trigger vertigo-so your brain learns they’re not dangerous. People who stick with it for 4-6 weeks see 70-80% improvement. But here’s the kicker: 30% quit early because the exercises make them dizzy at first. The good news? 95% of those who stick with it for two weeks feel dramatically better.What About Diet and Lifestyle?
If you have Meniere’s, sodium is your enemy. Too much salt = more fluid buildup = more vertigo. Doctors recommend 1,500 to 2,000 mg a day. That’s tough. A single bag of chips has 300 mg. A slice of pizza? 800 mg. You need to cook at home, skip processed foods, and read labels like your life depends on it. And it kind of does. Studies show people who stick to this diet cut their vertigo attacks by half.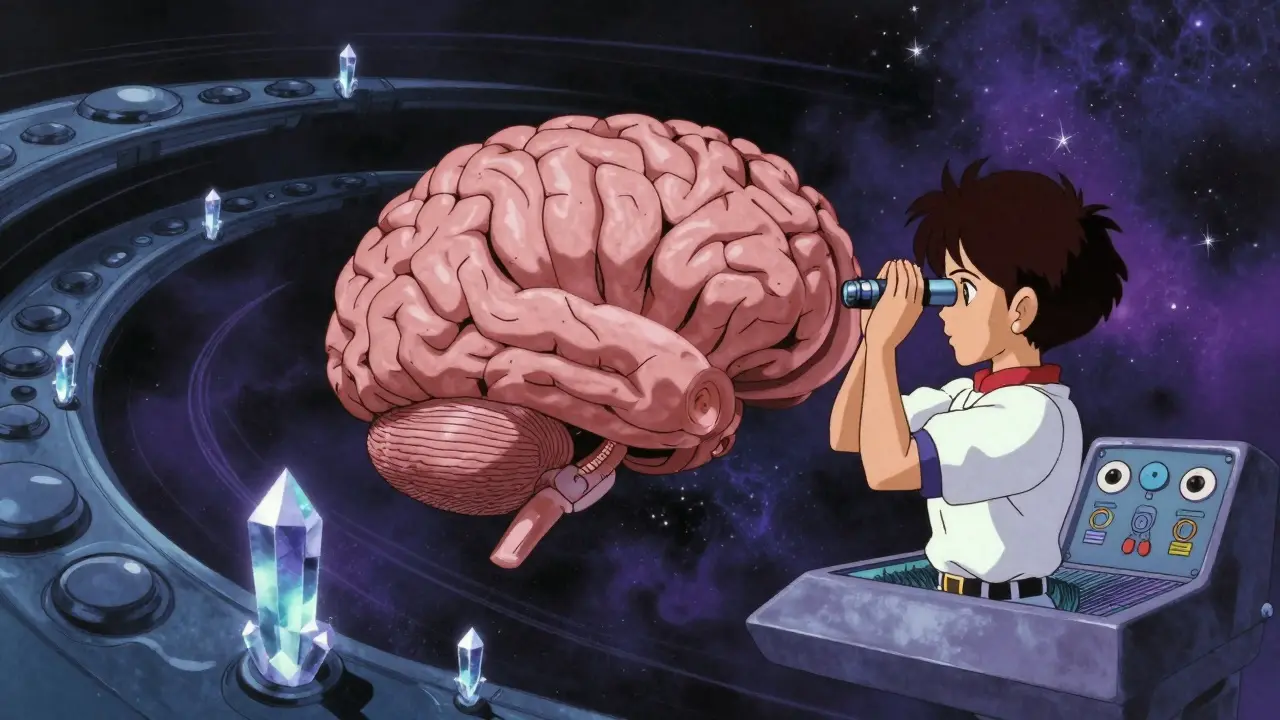
What About Migraines?
Vestibular migraine is the second most common cause of vertigo after BPPV. You don’t even need a headache. Just dizziness, light sensitivity, and nausea. Treatment? Migraine preventatives-meds like propranolol or topiramate. Not painkillers. Not anti-dizziness pills. The right meds can cut vertigo frequency by half. Keeping a daily diary of triggers-stress, sleep, food, weather-helps doctors find patterns. Most people find their triggers within four weeks.Real People, Real Results
One patient on Healthgrades said: “After three months of being told it was anxiety, the Epley maneuver fixed me in 15 minutes. I wish my doctor had known to test for this.” Another said: “Meclizine made me too sleepy to work. The exercises took three weeks, but now I’m back to hiking.”What’s New in 2026?
Smartphones are now part of the diagnosis. Apps like VEDA and VertiGo use your phone’s camera to detect tiny eye movements that signal BPPV. They’re 85% accurate. Telehealth lets you do the Epley maneuver with a therapist on video-even if you live in a rural town. And new drugs like eptinezumab (Vyepti) are now approved specifically for vestibular migraine. Research is even looking at gene therapy for Meniere’s. But the most powerful tool? Still vestibular rehab. It’s been working for 30 years. And it still works.What to Do Next
If you’re dizzy or spinning:- Don’t panic. Most causes are treatable.
- See a doctor within 48 hours if it’s sudden and severe-rule out stroke.
- Ask: “Could this be BPPV?” Request the Dix-Hallpike test.
- If you have hearing loss, ringing, or pressure, ask about Meniere’s.
- Stop taking anti-dizziness meds after 72 hours unless your doctor says otherwise.
- Ask for a referral to vestibular therapy. Don’t wait.
You don’t need to live with vertigo. Your brain can relearn balance. Your inner ear can heal. But you have to move-literally. The exercises are simple. The results? Life-changing.

Edith Brederode
January 20, 2026 AT 07:29OMG I had BPPV last year and the Epley maneuver was a GAME CHANGER 🙌 I was so scared to move my head, but after one session with my PT, I felt like I got my life back. No more meclizine! Just do the exercises, even if you feel dizzy at first - it’s worth it. 💪🫶
Nadia Watson
January 20, 2026 AT 08:25It is quite remarkable how many individuals continue to rely upon pharmaceutical interventions for what is fundamentally a biomechanical issue. The vestibular system, when properly stimulated through targeted rehabilitation, demonstrates an extraordinary capacity for neuroplastic adaptation. One must consider the long-term implications of pharmacological suppression versus functional retraining.
Shane McGriff
January 21, 2026 AT 10:34Let’s be real - most doctors don’t even know about the HINTS exam. I went to three docs before one actually asked if I had positional vertigo. I was like, ‘What’s that?’ Then they did the Dix-Hallpike and boom - BPPV confirmed. Epley maneuver took 12 minutes. I cried. Not from dizziness. From relief. Stop letting your PCP guess. Demand the test.
Paul Barnes
January 22, 2026 AT 18:31There is a grammatical error in the third paragraph: ‘inside each ear, there are three fluid-filled loops called semicircular canals. Tiny crystals, called otoconia, sit in a nearby sac.’ The sentence after should be capitalized, but it isn’t. Minor, but it undermines credibility.
pragya mishra
January 24, 2026 AT 03:25Why do you think only Americans care about this? In India, people just endure vertigo and call it ‘dizziness from stress’. No therapy, no tests. You need to be rich to get this kind of care. And even then, doctors here don’t know about VRT. You’re lucky you have access.
Andy Thompson
January 24, 2026 AT 16:26They don’t want you to know this, but the inner ear is controlled by the government’s secret 5G frequency array. 🤫📡 The crystals don’t just ‘drift’ - they’re being manipulated by satellite signals to make you fall so they can track your movements. Vestibular therapy? Nah. Faraday cage hat and salt lamps are the real fix. #Truth
Thomas Varner
January 25, 2026 AT 15:40Interesting. I had vestibular neuritis after a bad flu. Took six weeks to feel normal. I did the gaze stabilization every day. It sucked. I’d get nauseous every time I moved my head. But after week three? I could walk without holding the wall. Honestly? The worst part was the fear. Not the dizziness. The fear.
Art Gar
January 26, 2026 AT 11:36One must question the moral imperative of promoting physical therapy over pharmaceuticals when the latter generates greater revenue for the medical-industrial complex. One wonders whether the emphasis on vestibular rehabilitation is truly rooted in clinical efficacy, or merely in the financial disincentives of prolonged medication use. A troubling paradigm, indeed.
Renee Stringer
January 27, 2026 AT 04:30People who don’t stick with therapy are just lazy. If you’re too weak to do the exercises, you deserve to keep falling. I’ve seen it too many times - people give up after two days and blame the system. It’s not the system. It’s you.
Crystal August
January 28, 2026 AT 21:32Everyone’s so obsessed with ‘VRT’ like it’s the holy grail. What about the people who have it and still get dizzy? What about the ones who can’t afford PT? Or live in a trailer park with no access to specialists? You act like this is a one-size-fits-all solution. It’s not. You’re ignoring the real problems.
Courtney Carra
January 28, 2026 AT 22:17There’s a metaphysical layer here, isn’t there? The inner ear - that tiny, fluid-filled labyrinth - is not just a biological organ. It’s the seat of our orientation in the cosmos. When the crystals drift, are we not also losing our spiritual alignment? VRT isn’t just physical. It’s a ritual of reconnection. The body remembers what the mind forgets. And the mind… the mind is just the echo of the ear.
thomas wall
January 30, 2026 AT 08:20It is lamentable that the public discourse surrounding vestibular disorders has been reduced to a series of algorithmic tips and TikTok-friendly maneuvers. The profound neurological retraining required to restore balance has been commodified into a ‘quick fix’ culture. This is not progress. It is simplification masquerading as enlightenment.
Jacob Cathro
January 30, 2026 AT 23:12Bro… the whole post is just a glorified ad for vestibular PT clinics. They’re selling you a $200 session to do what you can YouTube for free. And don’t get me started on ‘eptinezumab’ - that’s just a fancy word for ‘we’re charging you $10K for a shot that makes you feel like a zombie’. Real talk? Do the Epley. Cut the salt. Stop scrolling. Your brain will thank you. 🤡