When you or someone in your home takes prescription or over-the-counter meds, side effects aren’t just possible-they’re common. About 70% of American adults take at least one medication daily. That means someone in your house is likely to experience an unexpected reaction: a rash, nausea, dizziness, or worse. A home emergency kit for medication side effects isn’t about panic. It’s about being ready when things go wrong before you can reach a doctor or pharmacy.
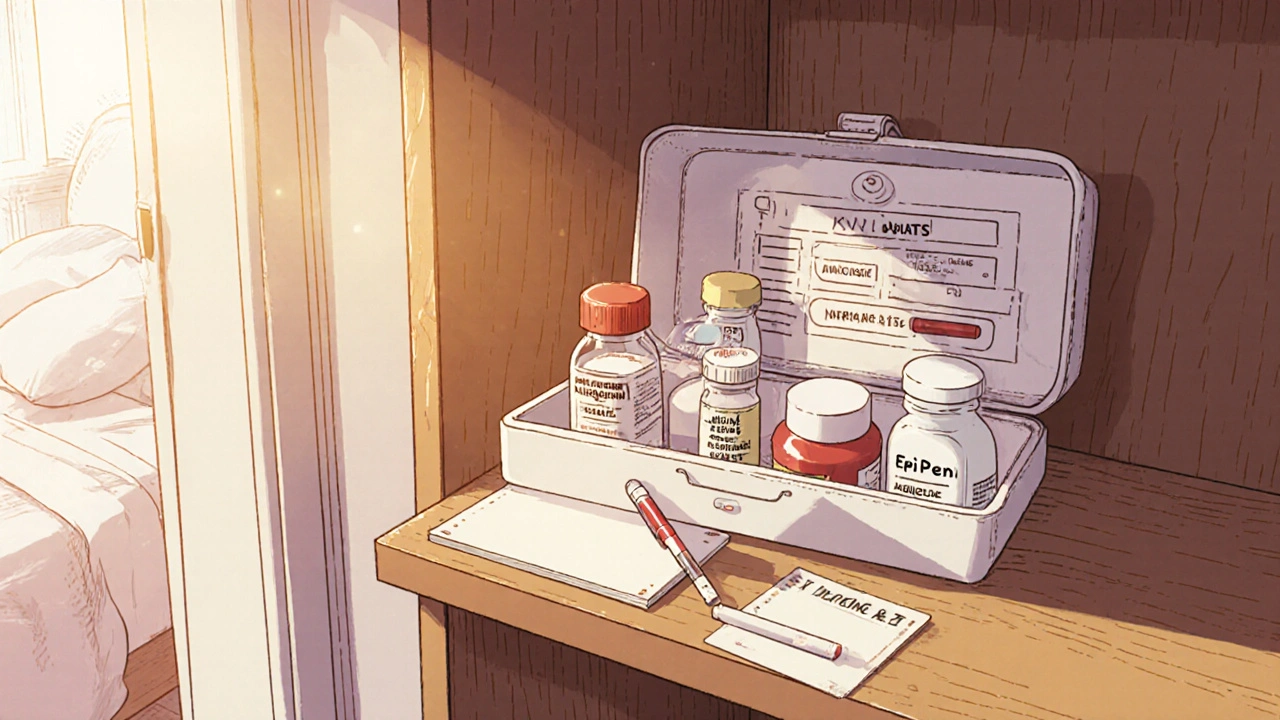
What Goes in the Kit? Start With the Basics
This isn’t your standard first-aid box with bandages and antiseptic. This kit is built for reactions caused by what’s inside your medicine cabinet. Here’s what you actually need:- Antihistamines like diphenhydramine (Benadryl) - for itching, hives, swelling, or trouble breathing from allergies. About 5-10% of people have some kind of allergic reaction to meds, and this can stop it before it gets serious.
- Hydrocortisone cream (1%) - for red, itchy skin rashes. Skin reactions make up 2-3% of all drug side effects. Keep a small tube in the kit so you can apply it right away.
- Antacids like Tums or Rolaids - for heartburn, upset stomach, or nausea. Up to 30% of people on certain meds get GI issues. Take them at the first sign of discomfort, not after it’s bad.
- Loperamide (Imodium) - for sudden, severe diarrhea. This is especially important if someone’s on antibiotics. About 25% of people on those meds get diarrhea, and dehydration can happen fast.
- Glucose tablets - for people taking insulin or diabetes meds. Low blood sugar can happen quickly from drug interactions. Keep 3-4 tablets in the kit so you can raise blood sugar fast.
- Epinephrine auto-injector (EpiPen) - only if prescribed. If someone has a history of severe allergic reactions to meds, this isn’t optional. Anaphylaxis can start in minutes. Don’t wait. Use it and call 911.
Don’t Forget the Paperwork
A kit without records is like a fire extinguisher without instructions. You need clear, printed info for every person in the household:- Medication list - name, dose, frequency, reason for use. Include both prescriptions and supplements. Use the 5 Rights: right patient, right drug, right dose, right route, right time.
- Allergy list - every drug, food, or substance that caused a reaction. Include symptoms (rash? swelling? trouble breathing?).
- Previous reactions - even if they happened years ago. Someone might forget they had a bad reaction to a painkiller in college. Write it down.
- Emergency contacts - your primary doctor, pharmacist, poison control (1-800-222-1222), and local ER. Put this on a card you can grab fast.
Include a small notepad and waterproof pen. Write down when the reaction started, what meds were taken, what symptoms appeared, and what you did. This helps doctors make faster, better decisions.
Storage Matters More Than You Think
You can have the best supplies in the world, but if they’re expired, wet, or in the wrong place, they won’t help.- Keep it cool and dry - not in the bathroom, not in the car. Heat and moisture ruin pills and creams. A drawer in the kitchen or bedroom is ideal.
- Out of reach of kids - 60,000 children end up in ERs each year from accidental medicine poisoning. Lock it if you have toddlers or curious teens.
- Check every 3 months - expiration dates aren’t suggestions. The FDA says meds can lose 10-50% of their strength before the date if stored poorly. Replace anything expired. Set a calendar reminder.
- Keep meds in original bottles - never dump pills into random containers. You need the label for dosage, expiration, and warnings.

What NOT to Include
Some things people think they need, they don’t. And some are dangerous.- Don’t give aspirin to kids - it can cause Reye’s syndrome, a rare but deadly condition. Use acetaminophen or ibuprofen instead, dosed by weight.
- Avoid activated charcoal - old guides said it helped with poisonings. Now, experts say it doesn’t work for most drugs and can delay real treatment.
- Don’t stock extra painkillers - especially acetaminophen (Tylenol). It’s in so many cold and flu meds. Taking extra can lead to liver failure. About 56,000 ER visits a year are from accidental overdose.
- Don’t include antibiotics - never use leftover antibiotics for new symptoms. They won’t help, and they can cause dangerous side effects or resistance.
Special Needs: Kids, Seniors, and Chronic Conditions
Your kit should fit your family, not a generic checklist.- For children - use weight-based dosing. Acetaminophen: 10-15 mg per kg. Ibuprofen: 5-10 mg per kg. Keep a small dosing syringe in the kit. No aspirin. Ever.
- For seniors - many take 4-5 meds daily. Include a simplified schedule with big print. Add a pill organizer with alarms if needed. Watch for interactions between blood pressure meds, diuretics, and heart drugs.
- For people on antidepressants or beta-blockers - stopping suddenly can cause dangerous withdrawal. Keep a week’s supply in the kit in case you’re stuck at home or the pharmacy is closed.
- For people with epilepsy or seizures - if a med triggers seizures, keep rescue meds like diazepam nasal spray if prescribed. Know how to use it.

When to Call 911 - and When Not To
This kit helps you manage, not fix. It’s a bridge to professional care.Call 911 if:
- Swelling of the face, lips, or throat
- Difficulty breathing or wheezing
- Chest pain or irregular heartbeat
- Loss of consciousness
- Seizure
Use your kit and call your doctor or poison control if:
- Skin rash or hives
- Mild nausea or diarrhea
- Headache or dizziness
- Low blood sugar (if you have diabetes)
75% of medication-related ER visits could have been avoided with better home management. That’s not just a statistic - it’s your family’s safety.
Talk to Your Pharmacist
Before you build your kit, sit down with your pharmacist. They know your meds better than anyone. Ask:- Which side effects are most likely for my meds?
- What OTC meds are safe to keep on hand?
- Do any of my meds interact dangerously?
- Can you print a simplified version of my med list?
Pharmacist advice reduces medication errors by 35%. That’s not a small number - that’s life-changing.
Make It a Family Habit
Don’t just build the kit. Practice with it.- Teach teens where it is and what’s inside.
- Review the list every time you refill prescriptions.
- Update it after a doctor changes a med.
- Check expiration dates together - make it a quarterly ritual.
Medication side effects don’t announce themselves. They show up when you’re asleep, on vacation, or in the middle of the night. A well-stocked, well-organized kit doesn’t just give you peace of mind. It gives you time - time to act, time to call for help, time to keep someone safe until professional care arrives.
Can I use my regular first-aid kit for medication side effects?
No. A standard first-aid kit is for cuts, burns, and sprains. Medication side effects need specific treatments like antihistamines, antacids, or glucose tablets. You need both kits - one for injuries, one for drug reactions.
How often should I check the expiration dates?
Every three months. Medications can lose potency before their printed expiration date, especially if stored in heat or humidity. Replace anything expired, even if it looks fine.
Is it safe to keep epinephrine at home?
Only if prescribed by your doctor. If someone has a history of severe allergic reactions to medications, an EpiPen can save their life. Keep it accessible, check the expiration date, and make sure everyone who lives with them knows how to use it.
Can I give my child Tylenol if they have a reaction to a medicine?
Only if you’re sure they haven’t taken another product with acetaminophen. Many cold, flu, and pain meds already contain it. Taking extra can cause liver damage. Always check labels and talk to your pharmacist first.
What if I don’t know what caused the reaction?
Call poison control at 1-800-222-1222. They’re available 24/7 and can help you identify the cause based on symptoms and meds taken. Don’t guess - get expert advice immediately.
Should I include painkillers in the kit?
Only if they’re part of your regular meds and you’re at risk of withdrawal. Don’t stock extra painkillers. They can lead to accidental overdose, especially with acetaminophen. It’s safer to use what you already have at home, with clear labels and dosing instructions.






Brad Seymour
November 7, 2025 AT 12:53Love this breakdown. I built a similar kit after my mom had a bad reaction to antibiotics-turned out she was allergic to the filler, not the drug itself. Now we keep antihistamines, hydrocortisone, and a printed med list in a locked Tupperware in the kitchen drawer. No more panic calls at 2 a.m. Just grab, read, act. Simple.
Malia Blom
November 9, 2025 AT 12:09Let’s be real-this whole ‘emergency kit’ thing is just capitalism repackaging common sense. You don’t need a $40 pre-packed box. You need a Google Doc and a pharmacy that doesn’t suck. Also, why are we still using EpiPens? They’re overpriced junk. Generic epinephrine auto-injectors exist. Stop paying for brand loyalty.
Erika Puhan
November 11, 2025 AT 06:04While the intent is commendable, the lack of pharmacoeconomic context undermines the entire framework. The reliance on OTC antihistamines without considering CYP450 enzyme interactions is a clinical oversight. Furthermore, the recommendation to store glucose tablets without addressing glycemic variability in polypharmacy patients is statistically negligent. This is not preparedness-it’s performative safety.
Edward Weaver
November 12, 2025 AT 11:08USA has the best meds in the world, and we’re still letting people buy stupid stuff like activated charcoal? We’re the only country that lets you walk into a store and buy diphenhydramine like it’s candy. You want a real emergency kit? Start by banning dumb supplements and forcing every pharmacy to print med lists in bold. Also, why is this even a debate? We’re Americans-we fix things.
Lexi Brinkley
November 13, 2025 AT 09:04OMG YES THIS!! 😭 I just used my kit last week when my cousin got hives from that new blood pressure med. Hydrocortisone + Benadryl = saved the day 🙌 Also, I printed my mom’s med list on neon pink paper so we can’t miss it. 💖 #MedSafetyQueen
Kelsey Veg
November 13, 2025 AT 10:21yea but like… what if u just forget to check the exp date? i had a benadryl that was 2 yrs out and it still worked? maybe the fda is just tryna sell more pills??
Alex Harrison
November 13, 2025 AT 23:45I’ve been using this setup since 2020. I keep the kit in the bedroom drawer with the epipen, antacids, and glucose tabs. I check it every 90 days like the article says. One time my kid had a reaction and we gave him the antihistamine before calling the doc. He’s fine. This isn’t hype-it’s just smart.
Jay Wallace
November 15, 2025 AT 17:37…And yet, the article fails to address the systemic failure of U.S. healthcare infrastructure-why must families bear the burden of pharmaceutical risk mitigation? The fact that we’re being told to stock epinephrine instead of fixing drug pricing, labeling, and provider communication is… profoundly dystopian. This isn’t preparedness. It’s damage control for a broken system.
Alyssa Fisher
November 16, 2025 AT 00:25What struck me most isn’t the items in the kit-it’s the emphasis on documentation. We treat meds like magic pills, but they’re chemicals with cascading effects. Writing down reactions? That’s not just helpful-it’s scientific. I started doing this after my aunt had a delayed reaction to a statin. We didn’t know it was linked until we had the timeline. Knowledge is the real emergency tool.
Alyssa Salazar
November 16, 2025 AT 21:50Let’s talk about the elephant in the room: polypharmacy in seniors. This kit is great, but it’s a Band-Aid. The real issue is that 40% of elderly patients are on 5+ meds with zero coordination between prescribers. If you’re giving grandma metoprolol, lisinopril, metformin, and a statin-she needs a pharmacist audit, not just a Tums tube. This kit helps manage symptoms, but the system is still failing her.
Beth Banham
November 18, 2025 AT 16:08My grandma has this kit. She doesn’t read the labels, but she knows where the pink box is. She opens it when she feels weird. I think that’s the whole point. It’s not about knowing everything-it’s about having something to do when you’re scared. And that’s enough.