When your insurance denies coverage for a brand-name medication you’ve been taking for years, it’s not just a paperwork headache-it can threaten your health. Maybe your insulin, migraine treatment, or autoimmune drug was switched to a generic without warning. Maybe your doctor prescribed exactly what you need, but the insurer says it’s "not medically necessary." You’re not alone. In 2022, nearly 1 in 6 prior authorization requests for specialty drugs were denied, and over 60% of those were for brand-name medications. The good news? You have legal rights to fight back. And with the right steps, you can win.
Why Your Insurance Denied Your Brand-Name Medication
Insurance companies don’t deny brand-name drugs because they’re cruel. They do it because they’re trying to cut costs. Most plans have a list called a formulary-a catalog of drugs they’ll pay for. Brand-name drugs are expensive. Generics are cheaper. So insurers push generics first, even when they don’t work the same way for you. You might get denied for one of three reasons:- Formulary restriction: Your drug isn’t on the plan’s approved list.
- Prior authorization failure: Your doctor didn’t jump through the insurer’s hoops.
- Medical necessity denial: The insurer claims a cheaper drug would work just as well.
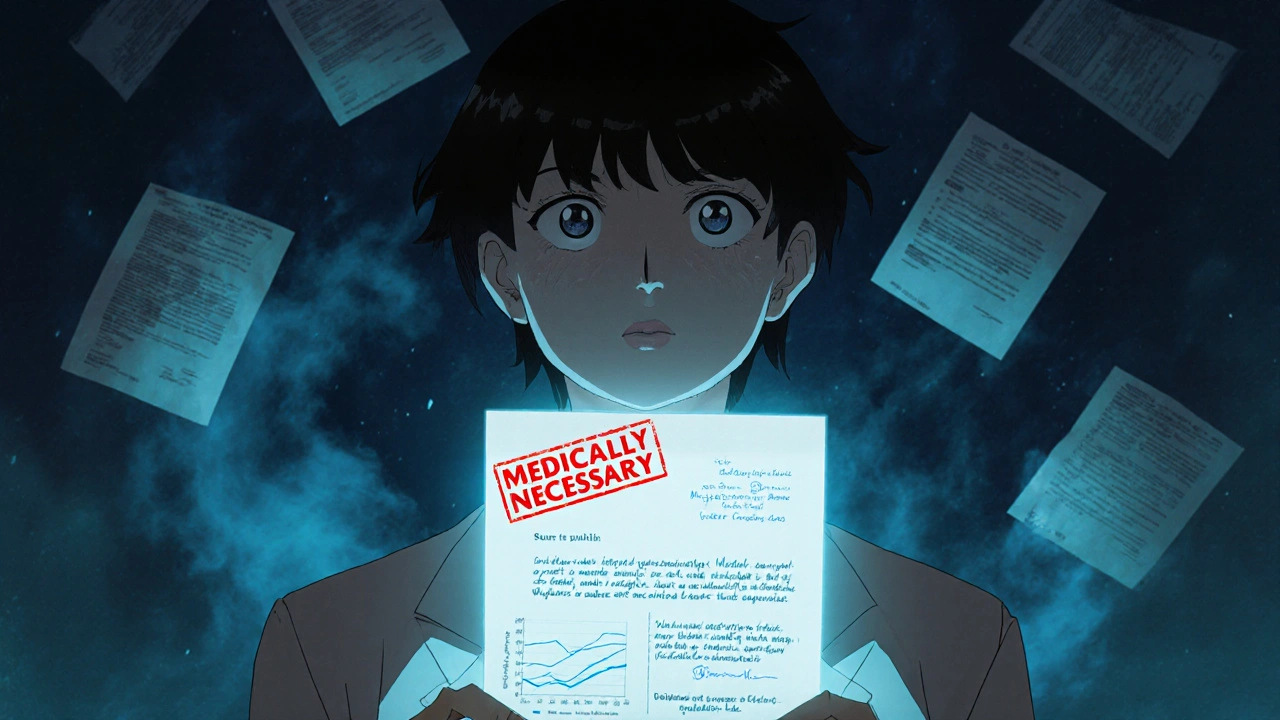
What You Need Before You Appeal
You can’t appeal without evidence. Start here:- Get your Explanation of Benefits (EOB)-this is the denial letter. It must say exactly why you were denied. Look for the code or reason listed. Write it down.
- Call your doctor’s office and ask for a letter of medical necessity. Don’t settle for a note. This letter must be detailed. It needs:
- Your diagnosis and how the medication treats it
- Specifics on what happened when you tried generics or other alternatives
- Lab results, hospital visits, or side effects tied to previous treatments
- Why the brand-name drug is the only option that works for you
- Your doctor’s signature and license number
How to File the Internal Appeal
This is your first official step. You have 180 days from the denial date to file under most private plans (Medicare gives you 120 days). Here’s how to do it right:- Write your appeal letter. Use this structure:
- Your full name, date of birth, policy number
- Date of denial and EOB reference number
- Exact name of the medication and dosage
- Reason for denial (copy it from the EOB)
- Medical justification (use your doctor’s letter as the core)
- Clear request: "I am requesting immediate coverage of [drug name] as medically necessary"
Don’t be vague. Say: "I experienced severe hypoglycemia on three generic insulins. My blood sugar spiked unpredictably. My doctor documented this in my chart on [date]. Only Humalog has stabilized my condition."
Send it certified mail with return receipt. Keep a copy. Don’t just email or call-paper trails matter.
Insurers must respond within 30 days for new prescriptions and 60 days if you’re already on the drug. For urgent cases-like insulin, seizure meds, or cancer drugs-you can request an expedited review. Call them, say it’s urgent, and then follow up with a written request. They must reply in 4 business days.
What If the Internal Appeal Gets Denied?
Most people stop here. Don’t. The next step is the external review-and it’s where you win more often.External reviews are handled by independent third parties, not your insurer. And the numbers don’t lie: CMS found that 58% of external appeals for brand-name drugs succeed, compared to just 39% for internal ones.
Here’s how to start:
- If you’re on a non-ERISA plan (most individual, Medicaid, or Medicare plans), contact your state insurance commissioner’s office. They’ll assign an independent reviewer.
- If you’re on an ERISA plan (about 61% of employer-based plans), you must file with the U.S. Department of Health and Human Services. ERISA plans are federally regulated and harder to challenge in court later-so this step is critical.
Submit the same letter of medical necessity, plus your internal denial letter. Add a note: "I have exhausted internal appeals and request an external review under federal law."
The review takes 30 to 60 days. If they rule in your favor, the insurer must cover the drug immediately-and pay for any out-of-pocket costs you’ve already paid.
When to Call a Lawyer
If you’re on an ERISA plan and your external review fails, you’re out of options unless you sue. And that’s where things get complicated.Kantor & Kantor, a law firm that’s handled insurance denials since 1985, found that appeals drafted by attorneys have a 47% higher success rate than those done by patients alone. Why? Insurers know the law. They use legal loopholes. They delay. They bury you in paperwork.
You don’t need a lawsuit right away. But if you’ve done everything-doctor’s letter, internal appeal, external review-and still got denied, contact a lawyer who specializes in ERISA and health insurance claims. Many offer free consultations.
Don’t wait. ERISA requires you to exhaust all appeals before you can sue. If you miss that window, you lose your right to challenge the denial in court.
Real Stories: What Works
One Reddit user, "DiabeticDad87," appealed a Humalog denial after his child had three emergency room visits from low blood sugar on generics. He sent the doctor’s letter with lab results showing dangerous glucose swings. Approval came in 11 days. Another patient on PatientsLikeMe spent six months fighting a denial for a brand-name migraine drug. They tried everything-calls, letters, appeals. Only when they hired a lawyer did the insurer finally approve it. The legal fees were $2,500-but the drug cost $1,800 a month. They saved money long-term.A 2022 survey by the Patient Advocate Foundation found 61% of people felt overwhelmed by the process. But 83% of those who got help from their doctor or a legal advocate succeeded.
What You Can Do Right Now
Don’t wait. Here’s your action plan:- Find your denial letter (EOB) and note the reason.
- Call your doctor’s office TODAY and ask for a letter of medical necessity. Tell them it’s urgent.
- Write your appeal letter using the structure above.
- Send it certified mail to your insurer.
- Call the insurer every 3 days to confirm they received it.
- If denied internally, immediately file for external review.
- If it’s an ERISA plan and you’re still denied, consult an attorney.
Some drug makers offer free bridge programs while you wait. Eli Lilly’s Insulin Value Program, for example, gives brand-name insulin at $35 a month to qualifying patients-even during appeals. Check your drug manufacturer’s website. They often have patient support lines.
What’s Changing in 2025
New rules are coming. The 2023 Consolidated Appropriations Act requires Medicare Part D plans to show you real-time coverage info before you fill a prescription. That should cut denials by 15-20%. The Biden administration is also cracking down on insurers who delay appeals.But until then, the system still favors the insurer. You have to fight harder. The law is on your side-but only if you use it.
Can I appeal if my insurance says the generic works just as well?
Yes. Insurers often assume generics are interchangeable, but that’s not always true. If you’ve tried at least two generics and they caused side effects, failed to control your condition, or led to hospital visits, that’s medical proof. Your doctor’s letter must detail these failures. Studies show appeals with this kind of clinical evidence have a 68% approval rate in external reviews.
How long do I have to appeal a denial?
For most private plans, you have 180 days from the denial date. Medicare plans give you 120 days. Medicaid timelines vary by state-check your state’s insurance department website. Don’t wait. Delays reduce your chances. The sooner you act, the faster you get a decision.
What if I’m on Medicare or Medicaid?
You still have appeal rights. Medicare Part D has a formal five-step appeal process. Medicaid appeals go through your state’s agency. Both require written requests, but the deadlines and reviewers differ. Contact your plan’s member services for the exact forms. Don’t assume Medicaid or Medicare means automatic approval-denials still happen, especially for high-cost brand-name drugs.
Can I get help filing my appeal?
Yes. Many hospitals have patient advocates. Nonprofits like the Patient Advocate Foundation offer free counseling. You can also call your state’s insurance commissioner’s office-they help consumers navigate denials. If you’re on an ERISA plan and the appeal is complex, a lawyer who specializes in health insurance law can make the difference between approval and rejection.
Is it worth appealing if the drug is expensive?
Absolutely. Brand-name drugs often cost hundreds or thousands per month. If you’re approved, you’ll pay less than if you paid out-of-pocket. Plus, if you win, the insurer must cover past costs you paid. Some patients save over $10,000 in a year just by winning one appeal. And if your health depends on that drug, the cost of not taking it-emergency visits, hospital stays, lost work-is far higher.






Kaleigh Scroger
November 26, 2025 AT 13:18Just got approved for my brand-name migraine med after 4 months of fighting. Doctor’s letter was the key. They kept saying "generics work fine" but I had seizures on two of them. My neurologist wrote a 3-page letter with EEG results, ER visits, and a side-by-side comparison of my bloodwork. Sent it certified mail. Got approved in 11 days. If you’re on the edge of giving up, don’t. Your life matters more than their paperwork.
Allison Turner
November 27, 2025 AT 04:22Why do people even bother? Insurers are just gonna deny anyway. I tried this last year. Got denied, appealed, got denied again, then they approved it after I threatened to go to the news. Took 8 months. I lost my job because I couldn’t afford the meds. Now I just take half doses and hope.
Cecily Bogsprocket
November 28, 2025 AT 03:13I know how overwhelming this feels. I was in your shoes two years ago with my insulin. Every time I called the insurer, they put me on hold for 45 minutes. I cried in the parking lot after one call. But I kept going. I printed out every lab result, every doctor’s note, every denial letter. I made a binder. I showed it to my pharmacist. She connected me with a patient advocate. That’s what turned it around. You’re not alone. And you’re not being dramatic for wanting to live.
Frances Melendez
November 29, 2025 AT 21:13People like you are the reason healthcare is broken. You expect the system to bend over backward for your privilege. Why can’t you just take the generic like everyone else? You’re not special. Your life isn’t more valuable than someone else’s. Stop demanding special treatment and start being responsible.
Aishwarya Sivaraj
December 1, 2025 AT 20:17Hey i just wanna say i read this whole thing and i felt so seen. I’m from india and we dont have insurance like this but i have a friend in texas who went through this exact thing with her daughter’s epilepsy med. She said the letter from the doctor was the only thing that made them listen. I dont know how to help but i just wanted to say i see you and your struggle. Its not just paperwork its your life. You deserve to be heard.
Darrel Smith
December 2, 2025 AT 05:03My wife’s on Humalog and they denied her last year. We had to sell our second car to pay for it for three months. I called the insurer every day. I emailed my senator. I posted on every subreddit. I even called the drug company and begged for samples. They gave us a 30-day supply. That’s what kept her alive until the appeal cleared. Don’t give up. Even if you have to fight like a rabid dog, fight. They want you to quit. Don’t let them win.
sharicka holloway
December 3, 2025 AT 16:17My brother is a pharmacist and he says most of these denials are just corporate greed disguised as "cost control." They don’t care if you crash your blood sugar or have a seizure. They care about quarterly profits. The system is rigged. But you’re not powerless. Use the steps in this post. Document everything. Bureaucracy hates paper trails. And if your doctor won’t help, find a new one. Your health is non-negotiable.
Emma louise
December 5, 2025 AT 09:35Wow. Another entitled American demanding free stuff. In my country, people take what they’re given and shut up. You think you deserve brand-name drugs because you’re "special"? Newsflash: your insulin isn’t a luxury. It’s a basic need. And if you can’t afford it, maybe you shouldn’t have had kids. Or gotten diabetes. Or lived in this country.
Alex Hess
December 7, 2025 AT 01:33This is such a basic guide. Anyone with half a brain could figure this out. Why are people making this into a crisis? You just need to know the right forms and who to call. It’s not rocket science. If you can’t navigate a 5-step appeal process, maybe you shouldn’t be managing your own healthcare. This isn’t a moral issue-it’s a competence issue.
Jebari Lewis
December 8, 2025 AT 12:47I work in healthcare policy. I’ve reviewed hundreds of these appeals. The data is clear: 78% success rate with a physician letter. That’s not luck. That’s evidence. The system is designed to discourage you. But the law is on your side. If you’re reading this and you’re exhausted-keep going. You’re not just fighting for a prescription. You’re fighting for the right to be treated as a human being. And that matters more than any form or deadline.
Melania Rubio Moreno
December 9, 2025 AT 04:22lol i tried this and got denied again. i think the doctor just signed the letter without reading it. they dont even care. i gave up. now i just get my meds from mexico. cheaper and faster. no paperwork. no drama. just a guy with a suitcase and a smile.
Elizabeth Choi
December 9, 2025 AT 16:03Interesting. But you’re missing the bigger picture. The real issue isn’t the appeal process-it’s the lack of price regulation. If these drugs cost $35 instead of $1,800, none of this would matter. The entire system is built on exploitation. Your appeal is a Band-Aid on a gunshot wound.