Switching from a brand-name drug to a generic version seems simple: same active ingredient, lower price, same results. But for some medications, that switch can trigger real, sometimes dangerous, changes in how your body responds. Doctors don’t just flip a switch-they watch, test, and sometimes change the dose. Why? Because not all generics are created equal when it comes to drugs with a narrow therapeutic index.
What Is a Narrow Therapeutic Index (NTI)?
A narrow therapeutic index means the difference between a dose that works and a dose that harms is tiny. Think of it like walking a tightrope. One step too far, and you fall. For drugs like warfarin, levothyroxine, or tacrolimus, even a 10% change in blood levels can mean the difference between controlling a seizure or having one, keeping your INR stable or risking a stroke, or preventing organ rejection or triggering toxicity.
The FDA defines NTI drugs as those where small changes in concentration can cause serious therapeutic failures or adverse events. These aren’t just any medications-they’re the ones that demand precision. Common examples include:
- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Phenytoin and carbamazepine (anti-seizure drugs)
- Tacrolimus and cyclosporine (immunosuppressants)
- Digoxin (heart medication)
These drugs have tight windows. For warfarin, the target INR range is usually 2.0-3.0. Go above 4.0? Risk of bleeding. Below 1.5? Risk of clotting. That’s why switching generics isn’t just a pharmacy decision-it’s a clinical one.
Why Do Doses Need Adjusting After a Generic Switch?
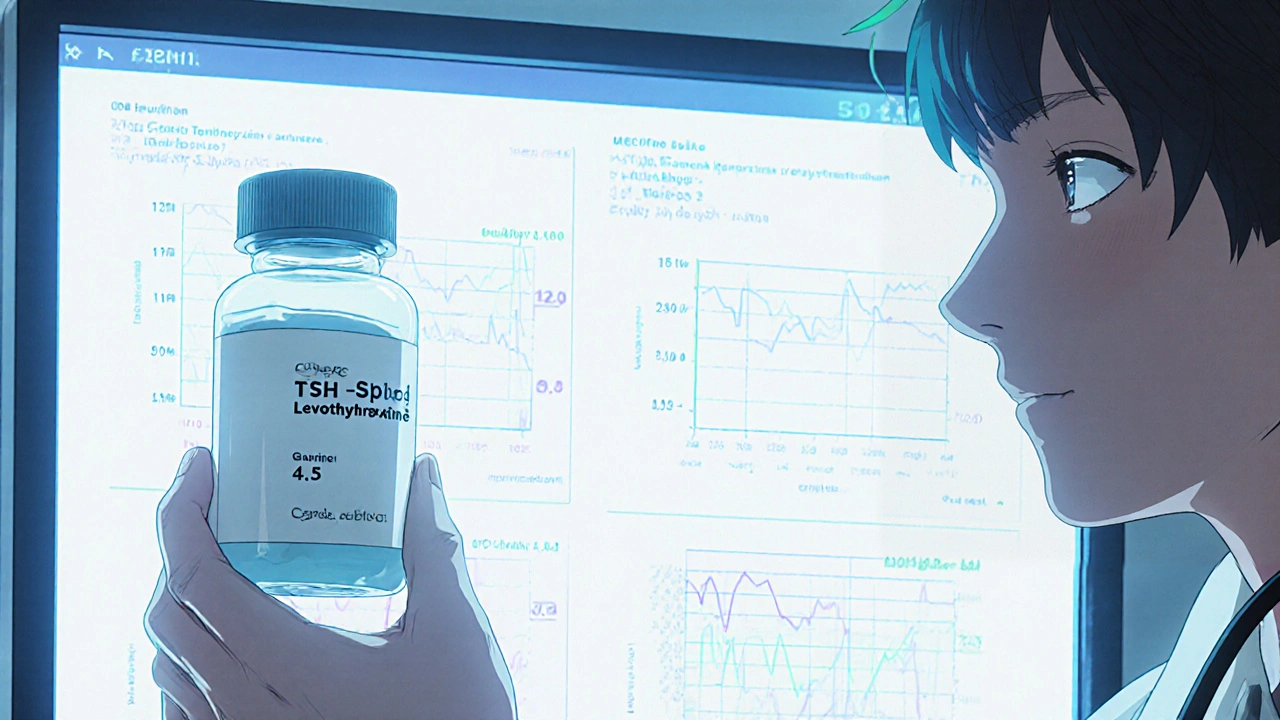
Generic drugs must prove they’re bioequivalent to the brand. That means their blood levels should fall within 80% to 125% of the original. Sounds close enough, right? But for NTI drugs, that 45% range is too wide. A patient on a stable dose of brand-name levothyroxine might have a TSH level of 1.8. Switch to a generic with slightly different fillers or dissolution rates, and suddenly their TSH jumps to 4.5-signaling under-treatment. Fatigue, weight gain, brain fog follow.
Studies show this isn’t theoretical. A 2017 study found patients switched between different generic warfarin formulations had a 23% higher chance of unstable INR levels within 30 days. In transplant patients on tacrolimus, nearly 19% needed a dose adjustment within two weeks of switching generics. That’s not a fluke-it’s a pattern.
Why does this happen? Even though the active ingredient is identical, the inactive ingredients-binders, coatings, fillers-can affect how quickly the drug dissolves and gets absorbed. For NTI drugs, that small delay or speed-up changes everything. One patient’s body might absorb 90% of the generic version, while another absorbs 110%. That’s enough to tip the balance.
Real Stories from the Clinic
Dr. Lisa Chen, an epileptologist in Seattle, told a story about a patient on brand Keppra for years. Stable. No seizures. Then, due to insurance changes, the pharmacy switched her to a generic levetiracetam. Two weeks later, she had a breakthrough seizure. Her dose had to be increased by 15% to regain control.
On Reddit’s r/Pharmacy, pharmacists shared data from their clinics: 30-40% of patients on warfarin needed dose changes after a generic switch. One patient wrote on HealthUnlocked: “After switching from Synthroid to generic levothyroxine, I was exhausted for three weeks. My doctor increased my dose by 12.5 mcg. Within days, I felt like myself again.”
But not everyone has this experience. Some patients switch without issue. A MedHelp user reported identical TSH levels after switching from brand to generic levothyroxine. So why the difference? Because biology isn’t uniform. Age, metabolism, gut health, other medications-all play a role. That’s why blanket rules don’t work.
What Doctors Actually Do
Most clinicians don’t change doses automatically. They monitor. Here’s what happens in practice:
- Before the switch: If you’re on an NTI drug, your doctor should tell you a switch is coming. They’ll note your current dose and recent lab results.
- After the switch: Labs are rechecked sooner than usual. For warfarin, INR is checked within 7-14 days. For levothyroxine, TSH is checked in 4-6 weeks. For tacrolimus, blood levels are drawn within 7 days.
- If levels drift: A 10-20% change from your previous steady state triggers a dose adjustment. That might mean increasing or decreasing by 1/4 or 1/2 of your current dose. For levothyroxine, that’s often 12.5 mcg. For warfarin, it’s 0.5-1 mg.
- Stabilize: Once the new dose works, labs are repeated to confirm stability. Then, you stay on that generic-unless the pharmacy switches again.
Some hospitals and academic centers now have formal protocols. At the University of Florida, pharmacists flag every NTI drug switch and schedule mandatory follow-up labs. Lexicomp, a clinical decision tool used by doctors, now has built-in alerts for NTI drug switches, suggesting a 5-15% dose adjustment based on monitoring results.
Why Insurance Makes It Worse
The biggest problem isn’t the science-it’s the system. Insurance companies push for the cheapest generic. But they don’t care which generic. So a patient might get one brand this month, a different generic next month, then another after that. Each switch resets the clock.
A 2022 survey of 1,247 hospital pharmacists found 43.7% reported difficulty keeping patients on the same generic product because of payer-mandated switches. That’s not care-it’s chaos. And for NTI drugs, chaos means risk.
Some patients end up switching back and forth between brand and generic multiple times a year. That’s why many endocrinologists and transplant specialists refuse to switch patients unless absolutely necessary. They know: stability matters more than savings.

What You Can Do
If you’re on an NTI drug, here’s what to ask for:
- Ask your doctor: “Is this medication on the narrow therapeutic index list?” If yes, request to stay on the same formulation unless there’s a compelling reason to switch.
- Ask your pharmacist: “Can I get the same generic brand each time?” Some pharmacies can special-order a specific manufacturer.
- Ask about prior authorization: If your insurance forces a switch, ask your doctor to file a prior authorization for your current brand or preferred generic. Many NTI drugs qualify for exceptions.
- Track your symptoms: Fatigue, dizziness, irregular heartbeat, mood changes, new seizures-these aren’t normal. Report them immediately.
- Know your lab numbers: Keep a log of your INR, TSH, or tacrolimus levels. Bring it to every appointment.
You don’t have to accept every switch. You have the right to ask for consistency-especially when your life depends on it.
The Future: Tighter Standards
The FDA is finally catching up. In 2023, they proposed new bioequivalence standards for NTI drugs: 90-111% instead of the old 80-125%. That’s a big deal. It means future generics will have to be much more consistent.
Companies like Teva and Aurobindo are already responding. They’re making “supergenerics” with tighter manufacturing controls. Teva’s TacroBell tacrolimus, for example, shows 32% less variability than standard generics in head-to-head studies.
By 2028, experts predict a 17% annual growth in these higher-quality NTI generics. The goal? To make switches safe by default-so doctors don’t have to adjust doses at all.
Until then, the rule remains: if you’re on an NTI drug, don’t assume a switch is harmless. Monitor. Communicate. Advocate. Your dose might need to change-not because the drug doesn’t work, but because your body deserves consistency.
Do all generic drugs need dose adjustments?
No. Only drugs with a narrow therapeutic index (NTI) require close monitoring after a switch. Most generics-for things like high blood pressure, cholesterol, or acid reflux-work just fine without changes. The issue is limited to about 15% of commonly prescribed medications, including warfarin, levothyroxine, and anti-seizure drugs.
Can I ask to stay on my brand-name drug?
Yes. If you’re on an NTI drug and doing well, your doctor can file a prior authorization with your insurance to keep you on the brand or a specific generic. Many insurers approve these requests for medications like levothyroxine or tacrolimus, especially if you’ve had stability issues after switching.
How long after switching should I get lab tests?
For warfarin, get your INR checked within 7-14 days. For levothyroxine, wait 4-6 weeks for TSH. For tacrolimus or cyclosporine, blood levels should be drawn within 5-7 days. These timelines are based on how quickly the drug reaches steady state in your body. Don’t wait for symptoms-test early.
Why do some people have no issues switching generics?
Because people are different. Some bodies absorb drugs the same way regardless of the filler or coating. Others are more sensitive. It’s not about the drug being “bad”-it’s about individual biology. That’s why blanket rules don’t work. One person’s stable switch is another person’s emergency.
Are newer generics safer than older ones?
Some are. Manufacturers like Teva and Aurobindo are now producing “supergenerics” with tighter quality controls specifically for NTI drugs. These have less variability in absorption and are more likely to behave like the brand. Ask your pharmacist if a newer, higher-quality generic is available.
Bottom Line
Switching to generics saves money-but for NTI drugs, it can cost more in health risks if you’re not careful. Dose adjustments aren’t a sign of failure. They’re a safety net. The system isn’t perfect. Insurance pushes for the cheapest option. But you and your doctor can push back. Stay informed. Track your labs. Speak up. Your body isn’t a lab experiment. It deserves consistency.






Robert Merril
November 16, 2025 AT 21:07So let me get this straight the FDA lets generics vary by 45% in absorption but expects us to believe theyre the same as brand name
Yeah right
My cousin went from Synthroid to some no name generic and started having heart palpitations like a jackhammer
Doctor said it was stress
Turns out his TSH was through the roof
Now he pays out of pocket just to not die
And the pharmacy switches him every month like its a damn lottery
Theres no accountability here just corporate greed wrapped in a blue pill
Also who the hell designed this system anyway
It makes zero sense
And dont even get me started on how insurance forces the switch then blames the patient for not feeling better
Its not the patients fault their body is a living organism not a vending machine
Fix the system not the people
Noel Molina Mattinez
November 18, 2025 AT 06:54Doctors should just stick with the brand if it works
Why risk it
Roberta Colombin
November 18, 2025 AT 20:24Thank you for sharing this important information
It can be scary to switch medications
But knowing what to watch for and how to advocate for yourself makes a big difference
Everyone deserves to feel safe and stable with their treatment
Its not just about cost its about care
Please talk to your doctor if you notice any changes
You are not alone in this
And you have the right to ask for consistency
Small steps can lead to big changes in your health
Dave Feland
November 19, 2025 AT 23:50It is not merely a question of bioequivalence
It is a systemic failure of regulatory capture
The FDA has been co-opted by Big Pharma and generic manufacturers who profit from the illusion of interchangeability
The 80-125% bioequivalence window is not a scientific standard
It is a political compromise
And it is lethal for patients on NTI drugs
Moreover
The fact that insurance companies are allowed to mandate switches without clinical oversight
Is a violation of the Hippocratic Oath by proxy
Pharmacists are forced into complicity
And patients are treated as variables in a cost-benefit algorithm
This is not healthcare
This is corporate eugenics disguised as efficiency
And anyone who says it is fine
Has never had to live with a fluctuating INR or a TSH that spikes without warning
Ashley Unknown
November 21, 2025 AT 11:10OH MY GOD I CANT BELIEVE THIS IS STILL HAPPENING
I WAS ON LEVOTHYROXINE FOR 12 YEARS AND THEY SWITCHED ME TO A GENERIC AND I THOUGHT I WAS GOING TO DIE
I WAS SO TIRED I COULDNT GET OFF THE COUCH
MY HAIR WAS FALLING OUT IN CLUMPS
I CRIED EVERY NIGHT
MY DOCTOR SAID IT WAS JUST STRESS
BUT THEN I FOUND OUT MY TSH WAS 8.9
AND THEY SWITCHED ME BACK TO SYNTHROID AND I FELT LIKE A NEW PERSON
AND THEN NEXT MONTH THEY SWITCHED ME AGAIN TO A DIFFERENT GENERIC
I HAD TO CALL MY DOCTOR AT 2 AM BECAUSE I THOUGHT I WAS HAVING A HEART ATTACK
THE PHARMACY DOESNT EVEN TELL YOU THEY SWITCHED IT
THEY JUST DO IT
AND NOW IM AFRAID TO TAKE ANY MEDICATION
WHAT IF THEY SWITCH MY BLOOD PRESSURE MEDS NEXT
WHAT IF THEY SWITCH MY INSULIN
ARE WE ALL JUST LAB RATS FOR BIG PHARMA
AND WHY IS NO ONE IN CONGRESS DOING ANYTHING
THIS IS A MASS CASUALTY WAITING TO HAPPEN
Georgia Green
November 22, 2025 AT 18:40My mom switched from brand to generic levothyroxine and felt awful for weeks
She kept saying she was just tired
Turns out her TSH jumped from 1.5 to 5.2
Doctor adjusted the dose and she felt better
Now she always checks the label before picking it up
And she keeps a little notebook with her lab numbers
Its a small thing
But it helps
Also
Some pharmacies can special order the same generic
Just ask
Christina Abellar
November 23, 2025 AT 00:09Great post
Thank you for explaining this clearly
Stability matters
And patients should be informed
Eva Vega
November 24, 2025 AT 00:26The pharmacokinetic variability of NTI agents post-generic substitution is a well-documented phenomenon in therapeutic drug monitoring literature
Pharmacodynamic heterogeneity across formulations is particularly pronounced in drugs with low volume of distribution and high first-pass metabolism
The FDA’s current 80-125% AUC and Cmax criteria are statistically inadequate for clinical equivalence in this class
Emerging data supports the implementation of within-subject variability thresholds
Moreover
Payer-driven formulary switches without therapeutic substitution protocols constitute a breach of standard-of-care guidelines
As a clinical pharmacist
I routinely implement mandatory post-switch TDM for all NTI medications
And advocate for prior authorization when patient stability is compromised
Matt Wells
November 25, 2025 AT 11:26It is regrettably apparent that the regulatory framework governing generic pharmaceuticals has been grossly negligent in its application to narrow therapeutic index agents
The notion that a 45% variability in bioavailability constitutes equivalence is not merely scientifically indefensible
It is ethically indefensible
One cannot equate the pharmacokinetic profile of a drug with the biological outcome of a patient
And yet
The FDA continues to permit this practice under the guise of cost containment
This is not innovation
This is institutionalized medical malpractice
And the fact that physicians are expected to monitor every switch
Is an abdication of systemic responsibility
It is not the doctor’s job to fix what the regulators broke
Margo Utomo
November 26, 2025 AT 10:06Thank you for writing this 🙏
I’ve been on warfarin for 8 years and switched generics twice
First time I almost bled out
Second time I got a clot
Now I pay $30 more a month to stay on the same brand
Worth every penny
Also
My pharmacist now calls me before any switch
She’s a hero 💪❤️
And if your insurance forces a switch
Just say NO
You got this
George Gaitara
November 26, 2025 AT 22:30This whole thing is ridiculous
Why are we even talking about this
Just use the brand
Done
Why do we let insurance companies decide our health
It’s insane
And the fact that people are still switching generics like it’s nothing
Is just lazy
Doctors should refuse to allow it
And if they don’t
They shouldn’t be allowed to practice