Getting the right amount of liquid medicine isn’t just about following the label-it’s about avoiding dangerous mistakes. Every year, thousands of children and adults receive too much or too little medication because the wrong tool was used to measure it. A liquid medication dosing error can lead to hospital visits, organ damage, or worse. The good news? Most of these errors are preventable with the right device, clear instructions, and a simple shift in how we think about measuring medicine.
Why Household Spoons Are a Dangerous Choice
You’ve probably heard it before: "Give your child a teaspoon of this." But a kitchen teaspoon isn’t a medical tool. It’s not calibrated. It’s not consistent. One person’s "teaspoon" might be 3 mL. Another’s might be 7 mL. That’s more than double the dose. A 2020 report from the Institute for Safe Medication Practices found that household spoons are responsible for about 40% of all liquid medication errors in children. Even worse, many parents don’t realize they’re using the wrong tool. They assume a spoon from the drawer is fine-until their child gets sick from an overdose. The FDA has been clear since 2011: don’t use teaspoons or tablespoons on labels. And since 2022, they’ve mandated that all new liquid prescriptions must use only milliliters (mL). But old habits die hard. In 2023, nearly 28% of liquid medications still had teaspoon labeling on the bottle. That’s a red flag.What Device Should You Use? The Data Doesn’t Lie
Not all dosing tools are created equal. Here’s what the research says about the most common options:- Oral syringes - Most accurate. For a 5 mL dose, 67% of users measured correctly with a syringe. Only 15% did with a cup. Error rates for syringes hover around 4% for small doses. They’re especially critical for doses under 5 mL, like infant antibiotics or seizure meds.
- Dosing cups - Common, but problematic. They’re often too big, have too many markings, and are hard to read at eye level. Parallax error-where the angle of your view distorts the liquid level-is the #1 reason people misread them. One study found 81% of cups had unnecessary lines that confused users.
- Dosing spoons - Better than kitchen spoons, but still unreliable. Accuracy varies by brand and how full you fill it. Error rates can hit 15%, far above the 10% safety threshold set by the USP.
- Droppers - Fine for tiny doses (under 2 mL), but become inaccurate above 5 mL. They’re also easy to spill or squeeze too hard.
Oral syringes win every time for precision. Yet, only 35% of pediatric prescriptions come with one. Why? Because most people think they’re hard to use. But that’s a perception problem-not a reality one.
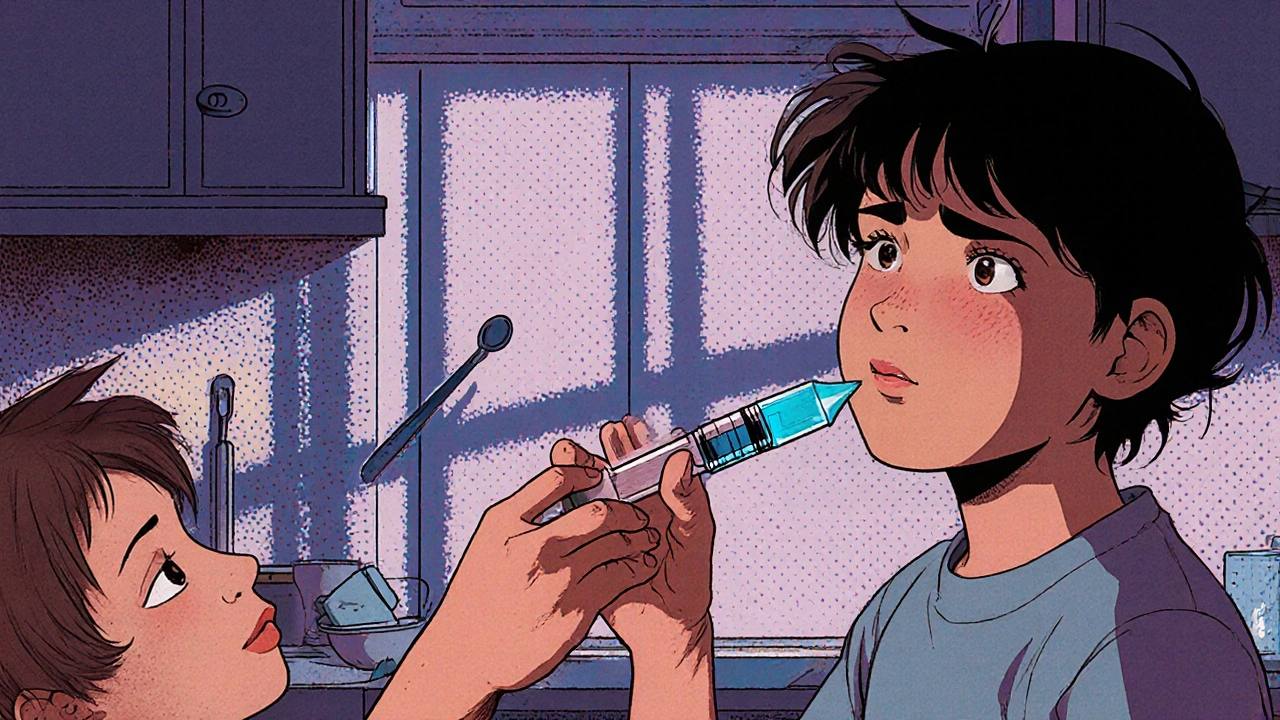
How to Use an Oral Syringe Correctly (Step by Step)
If you’ve never used one, it feels awkward. But with practice, it’s easier than a cup. Here’s how to do it right:- Wash your hands and the syringe tip.
- Draw up a little air-about 0.5 mL-by pulling the plunger back before inserting it into the bottle.
- Insert the tip below the liquid surface. Slowly pull the plunger to the exact dose mark. Don’t rush.
- Tap the side of the syringe gently to bring any air bubbles to the top, then push the plunger slightly to remove them.
- Hold the syringe level with your eyes. Read the dose at the top edge of the liquid (the meniscus). Never look from above or below.
- Give the dose slowly, aiming toward the inside of the cheek, not straight down the throat.
- Rinse the syringe with water after each use. Don’t let it dry out with medicine inside.
Practice with water first. Fill the syringe to the prescribed dose, then pour it into a measuring cup to check. If it’s off by more than 0.2 mL, try again. This takes 5 minutes-and could save a trip to the ER.

Label and Device Must Match-Exactly
Here’s a silent killer: mismatched labels and devices. The bottle says "5 mL," but the cup inside says "1 tsp." Or the label says "2.5 mL," but the syringe only has markings for 1 mL and 5 mL. That’s not a design flaw-it’s a safety failure. The National Council for Prescription Drug Programs (NCPDP) found that 89% of products have inconsistencies between the label and the included device. That’s almost every single one. Always check:- Is the label written in mL only? If you see "tsp," "tbsp," or "cc," ask for a new bottle or a new label.
- Does the device match the dose? If the prescription is for 1.6 mL, the syringe must have 0.1 mL markings. If it only has 1 mL and 2 mL lines, it’s not safe.
- Is there a leading zero? "0.5 mL" is correct. ".5 mL" is not. The FDA requires this to avoid misreading.
- Are there trailing zeros? "5.0 mL" is wrong. It should be "5 mL." Trailing zeros suggest precision that doesn’t exist and can cause confusion.
Pharmacists are required to provide a device that matches the label. If they don’t, ask for one. If they say they don’t have it, insist. Your child’s safety isn’t optional.
What Pharmacies Should Be Doing (And What They’re Not)
Community pharmacies are the last line of defense. But many still hand out cups with pediatric prescriptions. A 2022 audit of 10,000 prescriptions found:- 58% of prescriptions came with a dosing cup
- Only 35% came with an oral syringe
- 24% came with no device at all
That’s unacceptable. The American Pharmacists Association recommends giving an oral syringe for all doses under 10 mL. In hospital settings, that’s standard. In pharmacies? Not even close.
Some chains are catching up. CVS’s "DoseRight" program gives QR codes on labels that link to video tutorials. Walgreens now offers Bluetooth-enabled syringes that sync with an app to confirm dose accuracy. These aren’t gimmicks-they’re lifesavers.
If your pharmacy doesn’t offer a syringe, ask. If they say no, go elsewhere. You’re not being difficult-you’re being responsible.

Teach-Back: The One Skill That Prevents Errors
Doctors and pharmacists often assume caregivers understand. They don’t. A 2021 study in Patient Education and Counseling found that using the "teach-back" method cuts dosing errors by 35%. Here’s how it works:- Explain how to use the device.
- Ask the caregiver: "Can you show me how you’ll give this at home?"
- Watch them do it with water.
- Correct any mistakes on the spot.
- Confirm they can do it alone.
This takes less than 5 minutes. But it’s the difference between a safe dose and a dangerous one. If your provider skips this step, ask for it. Don’t leave without seeing it done correctly.
What to Do If You Made a Mistake
Accidents happen. You gave 2 mL instead of 1.5 mL. You used a kitchen spoon. You misread the line. Don’t panic. Don’t wait. Call your pharmacist or pediatrician. Tell them exactly what happened: what medicine, what dose, what device, and when. Most errors are minor and cause no harm. But some-especially with antibiotics, seizure meds, or heart drugs-can be serious. Keep a log: write down the date, time, dose given, and any symptoms. This helps your provider assess risk.Bottom Line: Precision Saves Lives
Liquid medication dosing isn’t about convenience. It’s about accuracy. Oral syringes aren’t "for babies"-they’re for anyone who needs exact doses. Milliliters aren’t "too technical"-they’re the only unit that doesn’t lie. If you’re giving liquid medicine:- Use an oral syringe for doses under 10 mL
- Never use a kitchen spoon
- Make sure the label and device match in mL only
- Practice with water before giving the real dose
- Ask for a syringe if one isn’t provided
- Use teach-back to confirm understanding
These steps aren’t optional. They’re the difference between healing and harm. And in medicine, that’s the only line that matters.






Ginger Henderson
November 26, 2025 AT 17:01Wow, another one of those ‘everyone’s doing it wrong’ posts. I’ve been using spoons for 20 years and my kids are fine. Maybe the real problem is overmedicating?
Gina Banh
November 27, 2025 AT 06:39Spoons are a death sentence for toddlers. I work in pediatrics. I’ve seen the ER logs. The data isn’t debatable - syringes save lives. If your pharmacy doesn’t give you one, demand it. No excuses. This isn’t opinion, it’s clinical fact.
Deirdre Wilson
November 29, 2025 AT 03:17I used to think the syringe looked like a sci-fi weapon… until my niece got her first antibiotic. Now I use it for everything - even my coffee creamer. It’s like magic for precision. Also, tapping the bubbles? Genius. Why didn’t anyone tell me this sooner?
Ryan C
November 30, 2025 AT 07:08Actually, the FDA doesn't mandate mL-only labeling - they recommend it. And the 28% stat? That’s from a single state survey, not national data. Also, droppers are fine for neonates - you’re overgeneralizing. And what about cost? Syringes aren’t free. Not everyone can afford them. 🤷♂️
Dan Rua
December 1, 2025 AT 16:53Love this. My pharmacist gave me a syringe with my kid’s amoxicillin last month. I didn’t even know to ask. Thanks for reminding me to be more proactive. Also - teach-back? I’m stealing that. My sister’s a nurse, she’ll love it.
Bethany Buckley
December 1, 2025 AT 19:48The epistemological crisis of liquid dosing is not merely a matter of measurement - it is a symptom of our alienation from the materiality of care. We outsource agency to pharmaceutical infrastructure, then blame the spoon. The milliliter is not a unit of precision - it is a colonial artifact of quantification that erases embodied knowledge. 🌿✨ Why must we surrender our intuitive grasp of volume to the tyranny of calibrated plastic? The human hand, the spoon, the pulse of care - these are not obsolete. They are sacred. 🙏
Albert Guasch
December 2, 2025 AT 15:50As a clinical pharmacist with 18 years in pediatric medication safety, I can confirm the data presented here is not only accurate - it is conservative. The 4% error rate with oral syringes is supported by multiple double-blind studies from the Journal of Pediatric Pharmacology. The 81% confusion rate with dosing cups? That’s from the 2023 NCPDP audit. And yes - trailing zeros on labels like '5.0 mL' are a documented cause of fatal overdoses in elderly patients on anticoagulants. The FDA’s 2022 guidance was a step, but enforcement remains patchy. Pharmacies must be held accountable. If your child’s medication comes with a cup - return it. Demand a syringe. And if they refuse - file a complaint with your state board of pharmacy. This isn’t about being careful. It’s about professional responsibility.
Jaspreet Kaur
December 3, 2025 AT 01:24Mqondisi Gumede
December 4, 2025 AT 17:41