Antibiotic Liver Injury R-ratio Calculator
How This Works
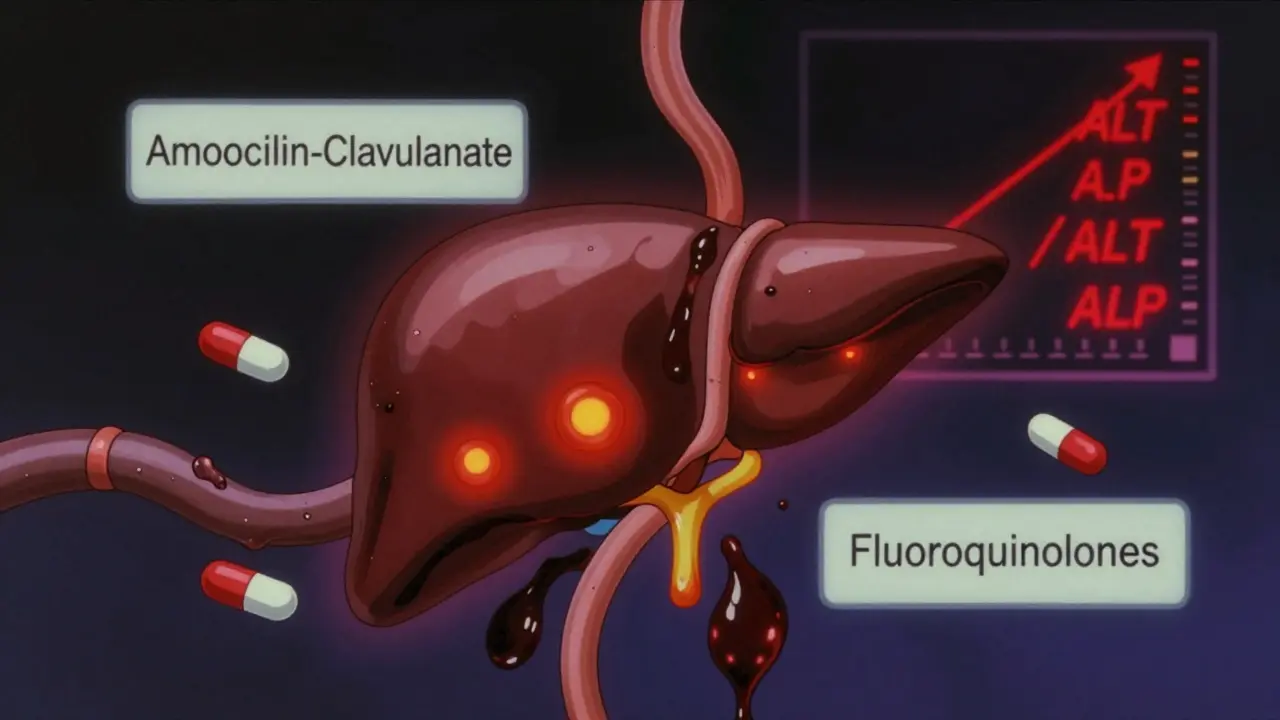
This tool calculates the R-ratio (ALT/ALP) to help identify if liver injury from antibiotics is hepatitis (ALT dominant), cholestasis (ALP dominant), or mixed injury.
When you take an antibiotic, you expect it to kill the infection-not harm your liver. But for some people, even common antibiotics can trigger serious liver damage. In fact, antibiotics cause 64% of all drug-induced liver injuries in the U.S., making them the number one culprit behind this often-overlooked side effect. If you’ve been on antibiotics for more than a week, especially in the hospital, your liver might be under stress-even if you feel fine.
How Antibiotics Hurt the Liver
Antibiotics don’t just target bacteria. They also mess with your body’s delicate balance, especially in the liver. There are two main ways this damage shows up: hepatitis and cholestasis.Hepatitis means your liver cells are getting damaged. This shows up as a spike in ALT (alanine aminotransferase), a liver enzyme. If ALT rises above 5 times the normal level, it’s a red flag. This pattern is common with antibiotics like isoniazid and fluoroquinolones.
Cholestasis means bile isn’t flowing properly. Your liver can’t get rid of waste, so alkaline phosphatase (ALP) and bilirubin build up. This is what you see with amoxicillin-clavulanate-the most common antibiotic linked to cholestasis. About 70-80% of cases with this drug show this pattern.
Doctors use something called the R-ratio to tell the difference. It’s just ALT divided by ALP, both adjusted to their normal limits. If the R-ratio is above 5, it’s hepatitis. Below 2? That’s cholestasis. Between 2 and 5? Mixed injury. This isn’t just academic-it changes how doctors respond.
Which Antibiotics Are Riskiest?
Not all antibiotics are created equal when it comes to liver damage. Some are far more dangerous than others.Amoxicillin-clavulanate (Augmentin) is the worst offender. It causes about 15 to 20 cases of liver injury per 100,000 prescriptions. That’s 10 times higher than fluoroquinolones like ciprofloxacin. It often hits 1 to 6 weeks after you start taking it, which is why people miss the connection-they think they’re past the side effects.
Tazobactam/piperacillin (Zosyn), a common ICU drug, is even scarier. In patients on it for 7+ days, nearly 29% develop liver injury. That’s almost 1 in 3. Compare that to meropenem, another ICU antibiotic, where the rate is only 12% under the same conditions.
Rifampin causes dose-dependent damage-more pills, more risk. And when it’s paired with isoniazid (used for tuberculosis), the liver toxicity jumps dramatically. Even nitrofurantoin and trimethoprim-sulfamethoxazole (Bactrim) are flagged as moderate-risk by the LiverTox database, despite being used for simple UTIs.
Gender matters too. Men are 2.4 times more likely than women to get liver injury from meropenem. Why? We’re still figuring it out, but it’s likely tied to how the liver metabolizes drugs differently between sexes.
Why Your Gut Matters
Your liver doesn’t work alone. It’s deeply connected to your gut. Antibiotics wipe out good bacteria, letting bad ones take over. This imbalance-called dysbiosis-breaks down your intestinal lining. Suddenly, toxins and bacterial parts leak into your bloodstream and head straight for your liver.Research shows people with low levels of Faecalibacterium prausnitzii, a key good gut bacterium, are 3.7 times more likely to develop antibiotic-related liver injury. That’s not a coincidence. This bacterium helps calm inflammation. When it’s gone, your liver gets bombarded.
Antibiotics also mess with mitochondria-the power plants inside your liver cells. They block energy production, flood cells with toxic chemicals, and trigger cell death. This is why some people develop sudden, severe liver failure even after taking a “safe” antibiotic for just a few days.
Who’s at Highest Risk?
It’s not just about the drug. Your health matters too.If you’re in the ICU with sepsis, your risk of antibiotic-induced liver injury goes up by 80%. Why? Your body is already under massive stress. Your liver is working overtime just to keep you alive. Adding antibiotics on top is like pouring gasoline on a fire.
People with pre-existing liver disease, older adults, and those on multiple medications are also more vulnerable. And here’s something many don’t realize: the longer you’re on antibiotics, the higher the risk. Taking them for 7 days or more triples your chance of liver injury compared to a 3-day course.
Genetics play a role too. Some people have HLA gene variants that make them extra sensitive to certain antibiotics. This explains why two people on the same drug, at the same dose, can have completely different outcomes-one fine, the other in the hospital.
How Doctors Spot It
The biggest problem? Liver injury from antibiotics looks a lot like other problems-viral hepatitis, gallstones, heart failure, or even worsening infection. In the ICU, it’s a diagnostic nightmare.Doctors rely on three things: timing, lab tests, and ruling out other causes.
- Timing: Did the liver enzymes rise after starting the antibiotic? Did they drop after stopping it? That’s the golden rule.
- Lab values: ALT > 5× ULN? ALP > 2× ULN with symptoms? That’s usually enough to stop the drug.
- Exclusion: No fever? No gallstones? No viral markers? Then it’s likely the antibiotic.
The LiverTox database from the National Institutes of Health is the gold standard for this. It tracks over 600 drugs and their liver effects. Amoxicillin-clavulanate? Score of 8-10 (high risk). Ciprofloxacin? Score of 4-5 (low to moderate). It’s not perfect, but it’s the best tool we have.
What Should You Do?
If you’re on antibiotics for more than a week, ask your doctor about liver monitoring. It’s simple: a blood test before you start, then again after 7 to 10 days. No cost, no pain, and it could save your liver.Watch for these signs: yellow skin or eyes, dark urine, extreme fatigue, nausea, or pain under your right ribs. Don’t wait. Call your doctor-even if you think it’s “just the infection.”
Don’t stop antibiotics on your own. But do speak up. If your doctor dismisses rising liver enzymes because “you’re just sick,” push back. This is real. And it’s preventable.
What’s Next?
The future is starting to look better. Researchers are testing probiotics to protect the gut during antibiotic therapy. Early results show promise. Clinical trials are also exploring genetic screening to identify people at high risk before they even take the drug.Some companies are building gut microbiome tests that can predict who’s likely to develop liver injury. Imagine getting a simple stool test before your antibiotic prescription-and knowing if you’re in the 1 in 5 group at high risk. That’s not science fiction. It’s coming within the next 5 years.
For now, the best defense is awareness. Antibiotics save lives. But they’re not harmless. Understanding how they affect your liver isn’t just for doctors-it’s for anyone who’s ever taken a pill for an infection.
Can antibiotics cause jaundice?
Yes. Jaundice-yellowing of the skin and eyes-is a classic sign of cholestatic liver injury caused by antibiotics like amoxicillin-clavulanate or rifampin. It happens when bile flow is blocked and bilirubin builds up in the blood. If you develop jaundice while on antibiotics, stop the drug and seek medical care immediately.
How long does it take for liver damage from antibiotics to show up?
It varies. For amoxicillin-clavulanate, symptoms usually appear 1 to 6 weeks after starting the drug. Fluoroquinolones like ciprofloxacin can cause injury in as little as 1 to 2 weeks. Some people don’t show signs until after they’ve finished the course. That’s why monitoring liver enzymes at 7 to 10 days is critical.
Are over-the-counter antibiotics linked to liver injury?
In the U.S., true antibiotics require a prescription. But some people misuse veterinary antibiotics or buy them online. These unregulated products can be contaminated or mislabeled, increasing liver injury risk. Even common OTC pain relievers like acetaminophen can worsen antibiotic-related liver damage. Always take antibiotics only as prescribed.
Can you recover from antibiotic-induced liver injury?
Most people do-especially if caught early. Stopping the antibiotic is the most important step. Liver enzymes usually return to normal within weeks to months. But in rare cases (less than 5%), the damage can be severe enough to require a liver transplant. Early detection saves lives.
Should I avoid antibiotics if I’m worried about my liver?
No. Antibiotics are life-saving when you have a serious bacterial infection. The goal isn’t to avoid them-it’s to use them wisely. Ask your doctor if the antibiotic is necessary, how long you really need it, and whether liver monitoring is recommended. For short courses (3-5 days) in healthy people, the risk is very low.
Is there a blood test to check for antibiotic liver damage?
Yes. A basic liver panel-ALT, AST, ALP, bilirubin, and albumin-is all that’s needed. No special test is required. If you’re on a high-risk antibiotic for more than 5 days, ask your doctor to order this test before and after your course. It’s the simplest way to catch damage early.






Himanshu Singh
December 29, 2025 AT 16:46Jasmine Yule
December 30, 2025 AT 09:25Greg Quinn
December 30, 2025 AT 19:00Lisa Dore
December 31, 2025 AT 02:40Sharleen Luciano
January 1, 2026 AT 22:22Jim Rice
January 3, 2026 AT 02:13Henriette Barrows
January 4, 2026 AT 11:18Alex Ronald
January 6, 2026 AT 07:07Tamar Dunlop
January 6, 2026 AT 18:18David Chase
January 7, 2026 AT 00:32Emma Duquemin
January 7, 2026 AT 03:54Kevin Lopez
January 8, 2026 AT 03:28Duncan Careless
January 8, 2026 AT 06:41Samar Khan
January 9, 2026 AT 22:03