Anticholinergic Burden Calculator
Assess your risk of cognitive decline from medications using the Anticholinergic Cognitive Burden (ACB) scale. This tool helps you understand how your current medications may impact your brain health.
Current Medications
Your Anticholinergic Burden Score
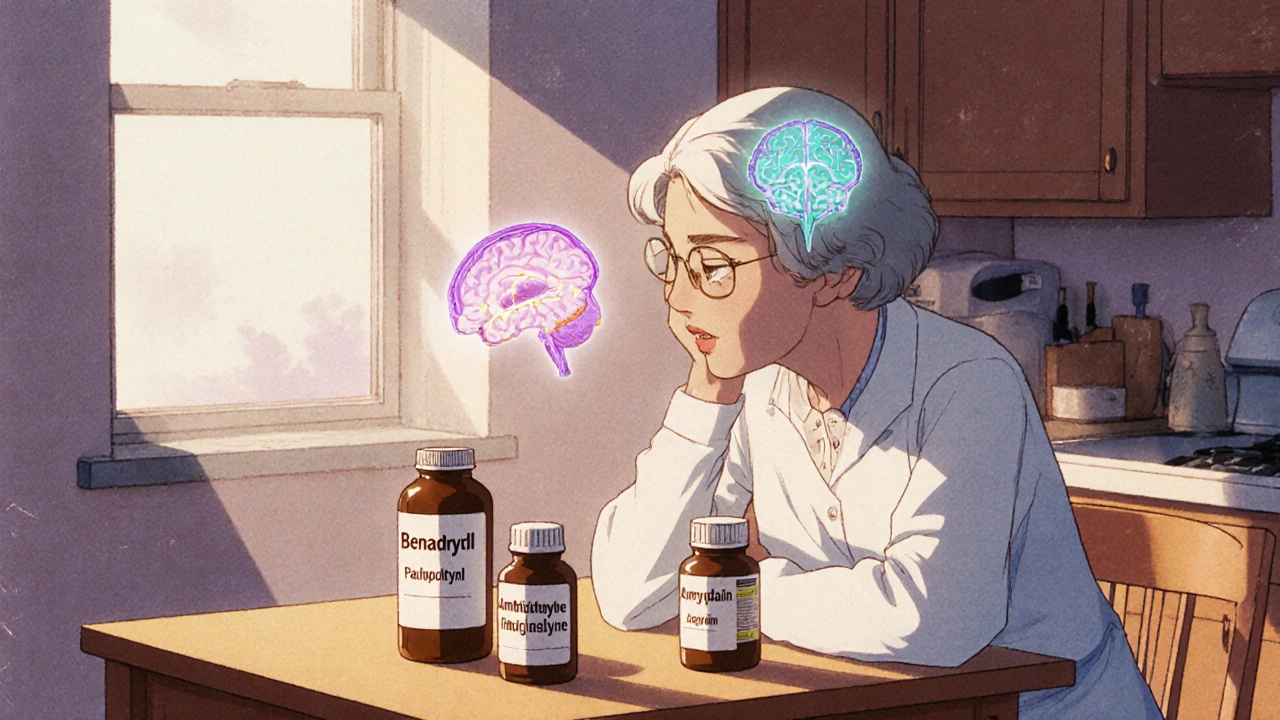
For years, millions of older adults have taken medications like Benadryl for allergies, oxybutynin for overactive bladder, or amitriptyline for nerve pain or depression. These drugs work. They relieve symptoms. But what if they’re quietly damaging your brain?
What Are Anticholinergic Medications?
Anticholinergic medications block acetylcholine, a key chemical in your brain and body that helps with memory, attention, muscle control, and even bladder function. These drugs have been around since the 1950s and are used for everything from motion sickness to Parkinson’s to chronic pain. Common ones include diphenhydramine (Benadryl), oxybutynin (Ditropan), tolterodine (Detrol), amitriptyline (Elavil), and even some sleep aids and stomach medications.
There are about 100 of these drugs on the market - many sold over the counter. That’s the problem. People don’t realize they’re taking something that can interfere with brain function. In the U.S., 10-15% of adults over 65 use at least one anticholinergic drug. That’s 15 to 20 million people.
The Link to Dementia Isn’t Theoretical - It’s Measured
Early studies suggested these drugs might cause temporary confusion. But newer research shows something more serious: long-term use is tied to actual brain changes and higher dementia risk.
A 2019 study using data from over 3,400 people found that those who took strong anticholinergics for three years or more had a 49% higher risk of developing dementia. That’s not a small increase. It’s comparable to the risk from smoking or uncontrolled high blood pressure.
Brain scans tell an even clearer story. People on these medications showed 0.5% to 1.2% more brain volume loss per year in areas critical for memory - the hippocampus and amygdala. Their brains also used less glucose, a sign of reduced activity. These aren’t random changes. They’re patterns seen in early Alzheimer’s disease.
And it’s not just one drug. The risk builds up over time. The more anticholinergic drugs you take - even weak ones - the higher your risk. This is called anticholinergic burden. Doctors now use tools like the Anticholinergic Cognitive Burden (ACB) scale to measure it. A score of 3 or higher on this scale is linked to measurable cognitive decline.
Not All Anticholinergics Are the Same
Here’s where things get tricky. Not every anticholinergic drug carries the same risk. Some cross the blood-brain barrier easily. Others don’t. That makes a huge difference.
For example:
- Tricyclic antidepressants like amitriptyline: Highest risk. One study found a 29% increased dementia risk.
- Bladder medications like oxybutynin and tolterodine: 20-23% higher risk.
- Antihistamines like diphenhydramine: Common in OTC sleep aids - moderate risk, but widely used.
- Trospium (for bladder issues): No significant link found. It doesn’t cross into the brain as easily.
That’s critical. If you’re on oxybutynin for bladder control, switching to trospium or mirabegron - both non-anticholinergic options - could cut your risk without losing symptom control.
Who’s Most at Risk?
It’s not just age. People with genetic risk factors - like the APOE-ε4 gene - are more vulnerable. So are those with existing memory issues, depression, or untreated sleep problems. The longer you take these drugs, the worse it gets.
One patient story from Reddit tells it plainly: “My mom was on amitriptyline for eight years. Her MMSE score dropped from 28 to 22 - a clear sign of decline. After stopping, it stabilized. But she never got back to where she was.”
That’s not rare. In patient forums, dozens report similar experiences. Yet, only 22% of users on Drugs.com mention cognitive side effects. Why? Because doctors don’t always warn patients. And patients don’t connect memory lapses to their nightly Benadryl.
Doctors Are Starting to Pay Attention - But Not Enough
The American Geriatrics Society has listed strong anticholinergics as drugs to avoid in older adults since 2019. The FDA added stronger warnings to 14 of these drugs in 2020. The European Medicines Agency restricted seven bladder drugs for elderly patients in 2021.
But here’s the gap: a 2021 survey found only 37% of primary care doctors routinely check for anticholinergic burden in patients over 65. Even though 89% say they know it’s risky, most don’t ask about OTC meds. They don’t check pill bottles. They don’t calculate burden scores.
Electronic health records now have built-in anticholinergic calculators - like those from Epic Systems - but most clinics don’t turn them on. Training takes time. Change is slow.
What Can You Do?
You don’t have to suffer silently. If you’re on one of these drugs, here’s what to do:
- Review all your meds - including OTC and supplements. Write them down. Bring the list to your doctor.
- Ask: “Is this drug anticholinergic?” If yes, ask: “Is there a safer alternative?”
- Don’t stop cold turkey. Some drugs cause withdrawal symptoms. Tapering takes 4-8 weeks.
- Ask about alternatives: For insomnia, try sleep hygiene or CBT instead of diphenhydramine. For depression, SSRIs like sertraline have near-zero anticholinergic activity. For overactive bladder, mirabegron or non-drug options like pelvic floor therapy work well.
- Track your memory. If you notice more forgetfulness, trouble focusing, or confusion, speak up. It might not be aging - it might be your meds.
One woman in her late 60s switched from oxybutynin to mirabegron. Her bladder symptoms stayed under control. Her memory improved. She started remembering names again. She didn’t realize her brain fog was tied to her bladder pill.
What’s Changing Now?
There’s momentum. The American Geriatrics Society launched the Anticholinergic Risk Reduction Initiative in 2022 with a goal to cut inappropriate prescribing by 50% by 2027. The Alzheimer’s Association estimates that reducing anticholinergic use could prevent up to 15% of dementia cases each year - roughly 570,000 people globally.
New drugs are coming. Seven bladder treatments and three antidepressants in late-stage trials are designed to avoid brain penetration. That’s good news. But they’re not here yet.
Right now, the safest choice is to avoid these drugs unless absolutely necessary. And if you need them, use the lowest dose for the shortest time.
It’s Not About Fear - It’s About Awareness
These medications aren’t evil. They help people with chronic pain, severe allergies, and overactive bladders. But they’re not harmless either. For older adults, the trade-off isn’t always worth it.
The science is clear: long-term use increases dementia risk. The tools to find out if you’re at risk exist. The alternatives are available. What’s missing is awareness - from patients and doctors alike.
If you’re over 60 and taking any of these drugs, don’t wait for a memory test to tell you something’s wrong. Ask your doctor now. Ask about alternatives. Ask about your brain.
Your memory might thank you later.
Can anticholinergic medications cause permanent memory loss?
Some people experience lasting cognitive changes after long-term use, especially with high-burden drugs like tricyclic antidepressants or oxybutynin. Brain scans show structural changes - like volume loss in memory centers - that may not fully reverse. Stopping the drug can stop further damage, but recovery isn’t guaranteed. Early action matters.
Is Benadryl safe for occasional use in older adults?
An occasional dose for allergies or a bad night’s sleep is unlikely to cause harm. But using it weekly or monthly over years adds up. Diphenhydramine is one of the most common sources of anticholinergic burden in seniors. Even low-dose, long-term use increases dementia risk. Safer sleep aids and non-sedating antihistamines like loratadine are better choices.
What’s the difference between oxybutynin and trospium for overactive bladder?
Oxybutynin crosses into the brain and has a high anticholinergic burden (ACB score of 3). Trospium doesn’t cross the blood-brain barrier easily and has a score of 1 or 0. Studies show oxybutynin raises dementia risk by 23%, while trospium shows no significant link. If you need a bladder drug, trospium or mirabegron are safer options.
Can I switch from amitriptyline to another antidepressant without worsening my pain?
Yes. Many people switch from amitriptyline to SSRIs like sertraline or SNRIs like duloxetine for nerve pain. These drugs have little to no anticholinergic effect and are just as effective for chronic pain in most cases. It takes 4-6 weeks to adjust, and your doctor should taper you slowly to avoid withdrawal. The cognitive benefit often outweighs the adjustment period.
How do I know if I’m taking too many anticholinergic drugs?
Use the Anticholinergic Cognitive Burden (ACB) scale. Each drug is assigned a score: 1 (mild), 2 (moderate), or 3 (strong). Add them up. If your total is 3 or higher, you’re at increased risk. Ask your pharmacist or doctor to calculate your burden. Many clinics now use EHR tools that do this automatically.
Are there any non-drug options for conditions treated with anticholinergics?
Yes. For insomnia: sleep hygiene, CBT-I, and avoiding screens before bed. For overactive bladder: pelvic floor exercises, timed voiding, and bladder training. For depression: exercise, therapy, and light therapy. For allergies: nasal saline rinses and HEPA filters. These aren’t magic fixes, but they work - and they don’t hurt your brain.
Is this risk only for people over 65?
Most research focuses on older adults, but the brain changes can start earlier. People in their 50s with long-term use show early signs of brain hypometabolism. The risk builds over decades. Reducing exposure in your 50s and 60s may help prevent decline later. It’s never too early to think about brain health.
What Comes Next?
If you’re taking one or more anticholinergic drugs, don’t panic. But don’t ignore it either. Schedule a med review with your doctor. Bring your pill bottles. Ask about your ACB score. Ask about alternatives. Ask about your brain.
There’s no single fix. But small changes - swapping one drug, cutting out nightly Benadryl, trying pelvic floor therapy - can add up. And for millions of people, that could mean keeping their memory, their independence, and their quality of life longer.






Shivam Goel
November 24, 2025 AT 20:17Let’s be real-this isn’t just about Benadryl. It’s about the entire medical-industrial complex treating aging like a bug to be suppressed, not a process to be understood. Oxybutynin? Sure. But what about the 37% of docs who don’t even check ACB scores? That’s not negligence-it’s systemic laziness. And don’t get me started on how OTC drugs are marketed like candy. You can’t just slap a ‘sleep aid’ label on diphenhydramine and call it harmless. The brain isn’t a vending machine. You don’t get to insert a pill and expect the same cognitive currency back.
Andrew Camacho
November 26, 2025 AT 11:13Look. I’m not here to sugarcoat this. I’ve seen my uncle go from fixing his own car to forgetting his own name-all because he was on amitriptyline for ‘nerve pain’ for 12 years. The science? It’s not speculative. It’s in the scans. The glucose uptake drops. The hippocampus shrinks. It’s not ‘getting old.’ It’s pharmacological erosion. And the FDA? They’re slow. But here’s the kicker: most people don’t even know their own meds have an ACB score. You want to live longer? Stop taking the stuff that’s literally eating your brain. Period.
Elise Lakey
November 27, 2025 AT 00:10I just read this and immediately checked my mom’s pill bottle. She’s been taking Benadryl every night for years. I didn’t realize it could be this serious. I’m scheduling a med review with her doctor next week. Thank you for writing this so clearly. I’m not scared-I’m motivated to act now.
Erika Hunt
November 27, 2025 AT 15:10It’s fascinating how deeply embedded these medications are in our culture-especially for sleep and bladder issues-and yet, we treat them like harmless conveniences. The fact that over 15 million older Americans are on these drugs without knowing the risks is terrifying. And yet, I’ve seen so many patients who say, ‘But it helps me sleep!’ or ‘My doctor said it was fine!’-and they’re not being negligent, they’re being misinformed. The system fails them because the warnings are buried in footnotes, not front-page headlines. We need public health campaigns-not just academic papers. Imagine a PSA: ‘Your nightly Benadryl might be stealing your memories.’ Would you still take it? I think most people would stop. The problem isn’t the drug-it’s the silence around it.
Shirou Spade
November 28, 2025 AT 02:59There’s a deeper philosophical layer here: we’ve outsourced our bodily autonomy to pharmaceuticals. We’ve forgotten that the human body isn’t a machine with replaceable parts. Acetylcholine isn’t just a neurotransmitter-it’s the very fabric of memory, presence, and identity. When we suppress it, we don’t just reduce symptoms-we reduce ourselves. The tragedy isn’t just the dementia risk-it’s that we’ve normalized cognitive erosion as ‘just part of aging.’ But it’s not. It’s preventable. And that makes it a moral failure.
Lisa Odence
November 29, 2025 AT 07:20OMG I JUST REALIZED MY MOM IS ON OXYBUTYNIN!!! 🤯🤯🤯 This is a PUBLIC HEALTH CRISIS!! The FDA should have banned these years ago!! I just checked her meds-ACB score is 4!! She’s 72!! She’s been on this for 7 years!! I’m calling her doctor TODAY!! And also, I’m starting a petition!! #StopAnticholinergics #BrainOverBladder 😭💊
Patricia McElhinney
November 30, 2025 AT 00:51Anyone who takes Benadryl nightly after 60 is asking for dementia. It’s not complicated. It’s not controversial. It’s basic neuropharmacology. And if your doctor doesn’t know the ACB scale? Fire them. And stop pretending OTC means safe. It means ‘unregulated’ and ‘unmonitored.’ You think your grandma’s forgetfulness is ‘just aging’? No. It’s a drug reaction. And if you’re still using diphenhydramine for sleep? You’re literally choosing brain decay over 8 hours of rest. Sad.
Agastya Shukla
November 30, 2025 AT 13:42There’s a critical distinction here between pharmacological burden and physiological adaptation. The anticholinergic effect isn’t inherently malignant-it’s the chronic, unmonitored exposure that shifts the equilibrium. The real issue isn’t the drugs per se, but the absence of longitudinal cognitive monitoring. We treat hypertension with regular BP checks-why not cognitive baseline assessments for seniors on polypharmacy? The tools exist. The infrastructure? Still in beta. We’re diagnosing dementia too late because we’re not measuring decline early enough.
giselle kate
December 1, 2025 AT 22:45Why are we letting Big Pharma get away with this? In the US, we let corporations sell brain-destroying drugs like candy. In Germany? They restrict these meds for seniors. In Japan? They use non-pharm approaches first. We’re not just behind-we’re complicit. This isn’t science. It’s capitalism. And until we stop treating older adults as profit centers, this will keep happening. Stop blaming patients. Blame the system that profits from their decline.
Karen Willie
December 3, 2025 AT 09:46I’m so glad this post exists. My aunt switched from oxybutynin to mirabegron last year. She didn’t think she’d notice a difference-but she started remembering birthdays again. She didn’t even realize she’d been forgetting them. Small changes matter. You don’t need to be perfect. Just start. Ask one question. Check one label. It’s never too late to protect your brain.
Leisha Haynes
December 4, 2025 AT 17:56Amy Hutchinson
December 5, 2025 AT 13:20