When you’re over 65 and managing diabetes, the goal isn’t just to lower blood sugar-it’s to stay safe. One bad low blood sugar episode can lead to a fall, a hospital trip, or even a heart attack. For seniors, hypoglycemia isn’t just uncomfortable-it’s life-threatening. And the medications meant to help can sometimes make things worse.
Why Seniors Are at Higher Risk for Low Blood Sugar
Your body changes as you age. Kidneys don’t filter drugs as quickly. Liver metabolism slows down. Hormones that normally kick in when blood sugar drops-like glucagon and epinephrine-don’t respond as strongly. That means even a small dose of diabetes medicine can push blood sugar too low, and your body won’t fight back like it used to. Plus, many seniors take multiple medications. The average person over 65 with diabetes is on nearly five prescription drugs and almost two over-the-counter ones. Some of those-like beta-blockers for high blood pressure or NSAIDs for joint pain-can hide the warning signs of low blood sugar or make diabetes meds work too hard. A heart rate that should spike during a low? Masked. Shaking or sweating? Overlooked as "just getting older."The Worst Culprits: High-Risk Diabetes Medications
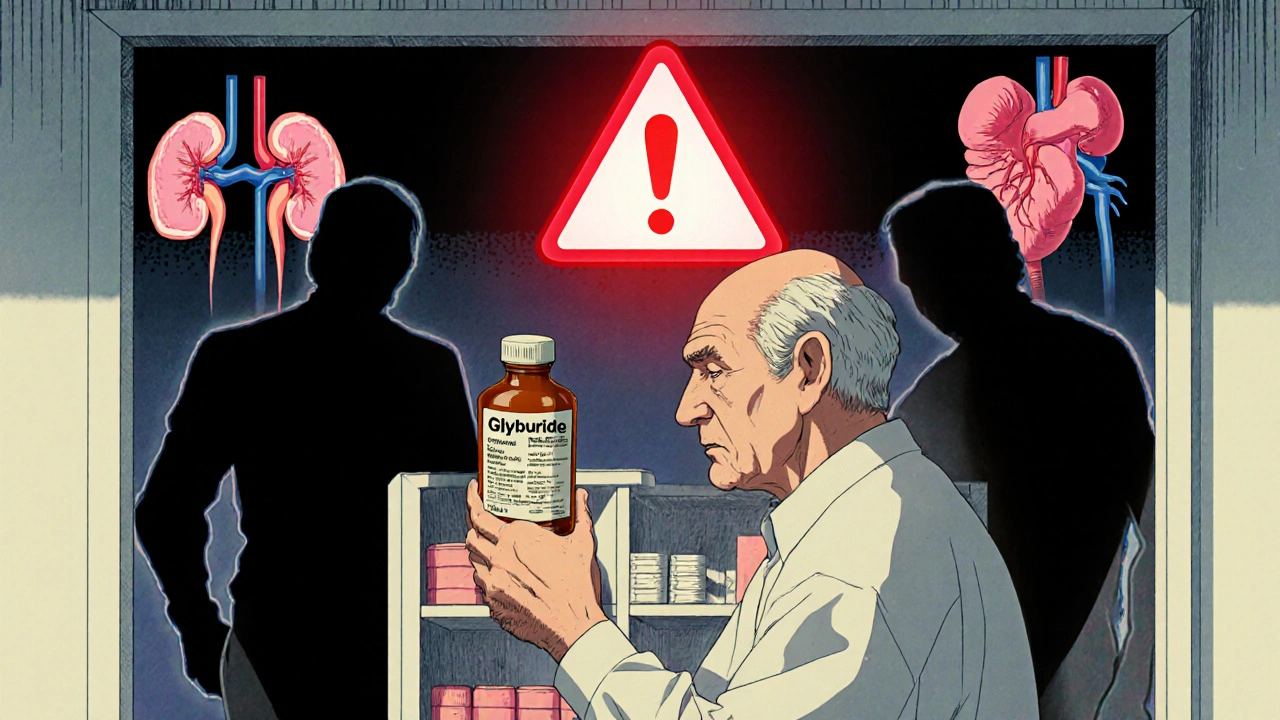
Not all diabetes pills and shots are created equal when it comes to safety. Some are far more dangerous for older adults. Glyburide (brand names: Glynase, Micronase) is one of the worst. It sticks around in the body way too long, especially in seniors with reduced kidney function. Studies show nearly 40% of elderly patients on glyburide have at least one hypoglycemia episode per year. One in five will have a severe low requiring emergency care. That’s why the American Geriatrics Society lists it as a medication to avoid in older adults. Glipizide (Glucotrol) is a little better-it clears faster from the body-but it still carries a 15-20% risk of low blood sugar in seniors. It’s not safe to assume it’s harmless just because it’s "less bad." Insulin, especially long-acting types like glargine or detemir, is another major risk. Seniors on insulin are 30% more likely to fall because of dizziness or confusion from low blood sugar. And insulin doesn’t care if you skip a meal or walk a little farther than usual-it keeps working, even when it shouldn’t.The Safer Alternatives: Medications That Won’t Crash Your Blood Sugar
The good news? There are much safer options now. DPP-4 inhibitors like sitagliptin (Januvia), linagliptin (Tradjenta), and saxagliptin (Onglyza) are among the safest choices. They work by helping your body use its own insulin more wisely-only when blood sugar is high. When used alone, they cause hypoglycemia in only 2-5% of seniors. Compare that to glyburide’s 30-40%. One 82-year-old man switched from glipizide to linagliptin and went from having nighttime lows every week to stable blood sugars between 90 and 140. SGLT2 inhibitors like empagliflozin (Jardiance) and canagliflozin (Invokana) also have very low hypoglycemia risk. They make your kidneys flush out extra sugar through urine. When used without insulin or sulfonylureas, they rarely cause lows. Clinical trials show hypoglycemia rates under 5%. Metformin is still a first-line choice for many, but it’s not risk-free. It doesn’t cause low blood sugar on its own-but if your kidneys aren’t working well, it can build up in your system. Doctors should check your creatinine clearance before prescribing it, especially if you’re over 80. And then there’s tirzepatide (Mounjaro), a newer injectable approved in 2022. In trials with seniors, it caused hypoglycemia in only 1.8% of users-far lower than insulin’s 12.4%. It’s not for everyone, but it’s a promising option for those who need stronger control without the danger.
What You Should Do: A Practical Action Plan
If you or a loved one is over 65 and on diabetes meds, here’s what to do right now:- Ask your doctor: "Which medication am I on, and is it safe for my age?" If you’re on glyburide, ask why-and if there’s a better option.
- Get your kidney function tested. A simple blood test (creatinine and eGFR) tells you if your body can clear meds properly. Many seniors have undiagnosed kidney decline.
- Review every pill you take. Bring a list of all medications-including vitamins and OTC drugs-to your next appointment. Some common ones, like ibuprofen or propranolol, can make hypoglycemia worse.
- Consider a continuous glucose monitor (CGM). These tiny sensors track your sugar 24/7 and alert you when it’s dropping. Seniors using CGMs cut their hypoglycemia events by 65% compared to fingersticks.
- Teach your family or caregiver the signs. Low blood sugar isn’t just shakiness. It can look like confusion, drowsiness, slurred speech, or even aggression. If someone’s acting "off," check their sugar.
Real Stories: What Happens When You Switch
Mary Thompson, 78, had three falls in six months. Each one started with a low blood sugar from glyburide. "I didn’t even feel it coming," she says. After switching to sitagliptin, she’s had zero lows in six months. "I walk my dog every morning now without fear." On Reddit, a caregiver wrote: "My dad was on glipizide and kept waking up in the middle of the night confused and sweaty. We thought it was dementia. Turns out, it was his medicine. After switching to linagliptin, he sleeps through the night for the first time in years." These aren’t rare cases. A 2022 study found that over 60% of emergency visits for medication problems in seniors with diabetes were due to hypoglycemia-and most were caused by sulfonylureas.
When to Say No to Tight Control
For younger people, doctors often push for an HbA1c under 7%. But for seniors, that goal can be deadly. The American Diabetes Association now recommends personalized targets:- 7.0-7.5% for healthy seniors with few other health problems
- 7.5-8.0% for those with multiple conditions but still active
- Up to 8.5% for frail seniors or those with dementia, heart failure, or other serious illnesses
What’s Coming Next
Scientists are working on "smart" insulins that only activate when blood sugar is high. Early trials are showing zero hypoglycemia in older adults. That’s not just promising-it could be revolutionary. For now, the best tools we have are knowledge and vigilance. Don’t assume older medications are fine just because they’ve been around for decades. The science has moved on. So should your treatment plan.What’s the safest diabetes medication for seniors?
The safest options for seniors are DPP-4 inhibitors like sitagliptin (Januvia) and linagliptin (Tradjenta), and SGLT2 inhibitors like empagliflozin (Jardiance). These rarely cause low blood sugar when used alone. Metformin is also safe if kidney function is normal. Avoid glyburide and long-acting insulin unless absolutely necessary.
Can diabetes meds cause falls in elderly people?
Yes. Low blood sugar from diabetes medications can cause dizziness, confusion, and weakness-leading to falls. Insulin and sulfonylureas like glyburide are the biggest culprits. Studies show seniors on insulin have a 30% higher risk of falling due to hypoglycemia.
How often should seniors get their diabetes meds reviewed?
Every 3 to 6 months. Seniors often develop new health issues or start new medications that can affect blood sugar control. Regular reviews help catch risks early and reduce the chance of dangerous lows.
Is metformin safe for seniors over 80?
It can be, but only if kidney function is good. Doctors should check creatinine clearance before prescribing it. Many seniors over 80 have reduced kidney function, which makes metformin risky. If kidneys aren’t working well, safer alternatives like DPP-4 inhibitors are preferred.
What should I do if I think my loved one is having a low blood sugar episode?
Check their blood sugar with a glucometer right away. If it’s below 70 mg/dL, give them 15 grams of fast-acting sugar-like 4 ounces of juice, 3-4 glucose tablets, or 1 tablespoon of honey. Wait 15 minutes and check again. If they’re confused, unconscious, or can’t swallow, call 911. Never give them insulin during a low.
Do continuous glucose monitors (CGMs) work well for seniors?
Yes, and they’re often more helpful for seniors than younger people. CGMs provide real-time alerts for rising or falling blood sugar, even overnight. Seniors using CGMs cut their hypoglycemia events by 65% compared to those using fingersticks alone. Many models have caregiver alerts so family members can step in if needed.






Richard Risemberg
November 20, 2025 AT 03:18Man, this post is a lifesaver. I’ve been watching my dad go through the wringer with glyburide-nighttime sweats, confusion, the whole nine yards. We switched him to linagliptin last year and it’s like he got his old self back. No more 3 a.m. panic attacks. He’s even started gardening again. Who knew a simple med switch could bring back someone’s joy? Seriously, if you’re on sulfonylureas, don’t wait till someone falls. Ask your doc today.
Chuck Coffer
November 21, 2025 AT 23:09So let me get this straight-you’re telling me the entire medical establishment has been poisoning old people for decades with cheap, outdated drugs because it’s cheaper than prescribing the new fancy stuff? And now you want us to believe this is just "science moving on"? Hmm. Tell me, who profits from Jardiance? Who owns the patents? Just asking.
Andrew Baggley
November 22, 2025 AT 02:33My grandma’s on metformin and her kidney numbers are borderline. Her doctor said "we’ll monitor." That’s not good enough. She’s 83, lives alone, and her CGM just saved her from a low last week. I’m pushing for her to switch to sitagliptin. If you’re not using a CGM for an elderly diabetic, you’re playing Russian roulette with a glucometer. Seriously. Get the sensor. It’s not expensive anymore. It’s not a luxury-it’s insurance.
Frank Dahlmeyer
November 22, 2025 AT 07:05I’ve been a nurse for 32 years and I’ve seen this exact scenario play out a hundred times. Elderly patient comes in with "dementia"-turns out it’s hypoglycemia from glyburide. Family thinks it’s aging. Doctor blames it on "cognitive decline." Meanwhile, the real villain is a $0.10 pill that’s been around since the 70s. The system is broken. We prioritize cost over care. We don’t re-evaluate meds unless something blows up. And when it does? It’s too late. This post should be mandatory reading for every geriatrician. And every family member. And every pharmacist. And every damn insurance rep who denies CGMs because they "aren’t medically necessary."
It’s not about saving money. It’s about saving dignity. And sleep. And walking without fear.
Andrew Montandon
November 22, 2025 AT 08:06Wait-so you’re saying insulin isn’t always the answer? And that DPP-4 inhibitors are safer? I’ve been told for years that insulin is the gold standard! I’m confused. Is this some kind of conspiracy? Are Big Pharma pushing these new drugs because they’re more profitable? Or is this actually legit? I’ve got my mom on insulin and she’s had two lows this month. I’m scared. I need to know-can I trust this? Can I really switch her? What do I even say to her doctor?
Michael Petesch
November 24, 2025 AT 02:40While the clinical data presented is largely accurate and aligns with current ADA guidelines, one must acknowledge the broader sociomedical context. The overprescription of sulfonylureas in geriatric populations reflects systemic underinvestment in geriatric pharmacology training, coupled with entrenched prescribing habits among physicians trained in an era where glycemic targets were uniformly aggressive. Furthermore, the disparity in access to newer agents like SGLT2 inhibitors and CGMs is not merely a clinical issue-it is a socioeconomic one. Many seniors, particularly in rural or underserved communities, cannot afford these technologies, even with insurance. Thus, while the therapeutic alternatives are commendable, their utility remains contingent upon equitable healthcare infrastructure-a factor rarely addressed in patient-facing educational content.
Codie Wagers
November 24, 2025 AT 19:16Let’s be honest: this isn’t about safety. It’s about control. The medical establishment wants you dependent on devices, on monitoring, on frequent appointments, on expensive drugs with side effects no one talks about. They profit from your fear. They profit from your confusion. They profit from your inability to say no. And now they’re selling you a CGM like it’s a miracle. It’s not. It’s a Band-Aid on a bullet wound. The real solution? Stop medicating elderly people with chemicals that were never meant for their aging bodies. Let them eat real food. Move gently. Sleep. Stop chasing numbers. Let nature take its course. You don’t need a doctor to tell you how to live. You just need to stop listening to them.
Sam Reicks
November 25, 2025 AT 12:19gotta love how they never mention the real cause of all this-vaccines. the jab messed up everyone's metabolism. my uncle was fine on metformin till he got his second booster. now he's on insulin and falling all the time. the docs wont admit it but its the nano tech in the shot. theyre hiding it. dont trust the pharma bots. check your blood sugar before and after the jab. youll see the spike. its not the meds. its the poison in the needle.