For millions of older adults, a small white pill labeled benzodiazepines has been a go-to solution for anxiety, trouble sleeping, or panic attacks. But what many don’t realize is that these drugs-commonly prescribed as Xanax, Valium, or Ativan-are now considered one of the riskiest medication classes for people over 65. The data is clear: the dangers far outweigh the short-term benefits, and safer options exist.
Why Benzodiazepines Are Riskier for Seniors
Benzodiazepines work by boosting GABA, a calming neurotransmitter in the brain. That sounds helpful, right? But in older adults, the body doesn’t process these drugs the same way it did in younger years. Liver function slows down. Kidneys filter less efficiently. And the brain becomes more sensitive to sedation. This means even low doses can lead to serious side effects.
Studies show that seniors on benzodiazepines are at least 50% more likely to suffer a hip fracture. Why? The drugs cause dizziness, poor balance, and delayed reaction times-exactly what you don’t want when walking across a slick kitchen floor or climbing stairs. One study of over 43,000 people found that those taking benzodiazepines had a risk of falling and breaking a hip similar to someone driving with a blood alcohol level of 0.06%. That’s legally impaired in most states.
Then there’s the brain. Long-term use is linked to memory loss, confusion, and even an increased chance of developing Alzheimer’s. A 2023 analysis from French and Canadian researchers found that seniors who took benzodiazepines for 3 to 6 months had a 32% higher risk of dementia. For those on them longer than six months? The risk jumped to 84%. And here’s the kicker: cognitive decline didn’t reverse even three months after stopping the medication.
These aren’t theoretical risks. They’re real, documented, and growing. The American Geriatrics Society’s Beers Criteria-used by doctors nationwide to guide safe prescribing-has listed benzodiazepines as potentially inappropriate for older adults since 2019. And the 2024 update made it even clearer: all benzodiazepines, no matter how short-acting, carry serious risks for seniors.
The Hidden Cost of “Just One Pill”
Many older adults start benzodiazepines after a stressful event-a death in the family, a move to a new home, or trouble sleeping after surgery. Their doctor says, “Try this for a few weeks.” But “a few weeks” often turns into months, then years. Why? Because stopping is harder than starting.
Withdrawal symptoms are real and often misunderstood. When someone stops benzodiazepines suddenly, they can experience rebound anxiety, insomnia, tremors, nausea, and even seizures. That’s why tapering is essential. But many doctors don’t have the time or training to guide patients through it. A 2024 guideline from the American Society of Addiction Medicine recommends reducing the dose by 5-10% every one to two weeks. For some, that takes 6 to 12 months.
And then there’s the emotional barrier. Patients often believe the medication is the only thing keeping them calm. A Reddit post from a geriatric nurse in March 2024 said, “Nine out of ten elderly patients I see think their Xanax is completely safe because their doctor prescribed it.” That trust is understandable-but dangerous.
What Works Better Than Benzodiazepines?
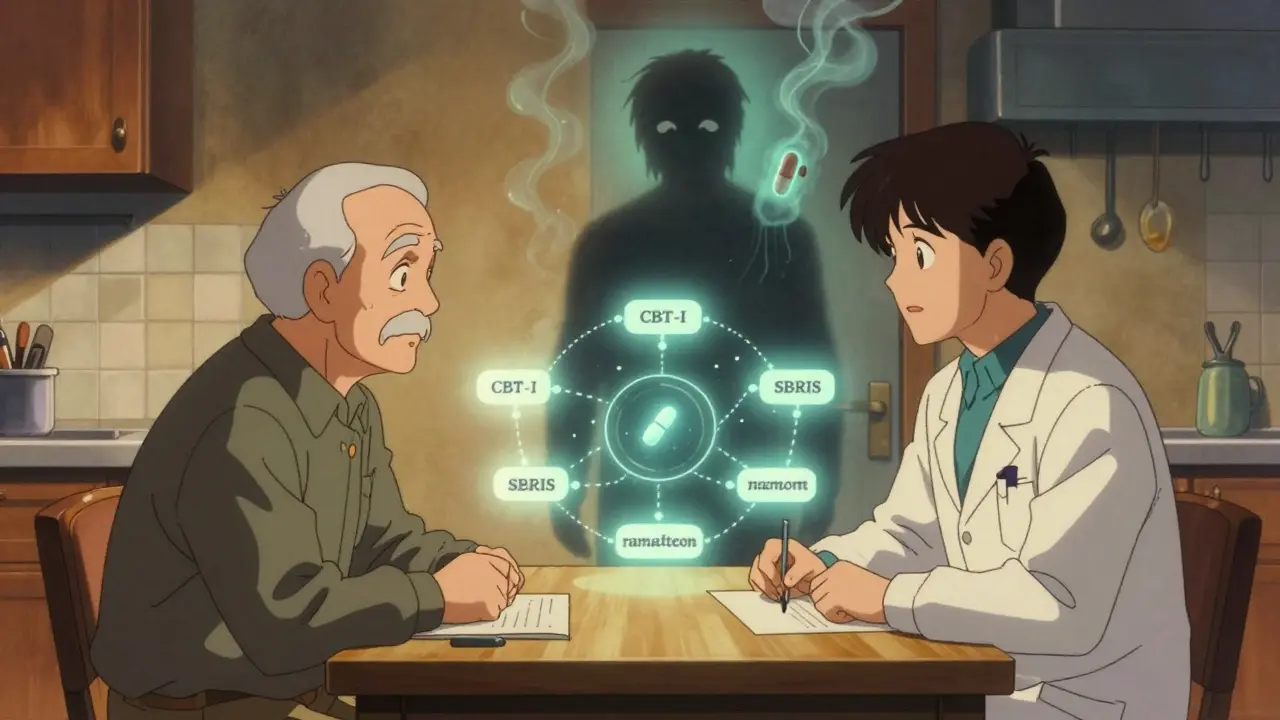
The good news? There are safer, more effective ways to manage anxiety and insomnia in older adults.
Cognitive Behavioral Therapy for Insomnia (CBT-I) is the gold standard. It’s not a pill. It’s a structured program that helps retrain your brain around sleep. Studies show 70-80% of seniors who complete CBT-I see major improvements in sleep quality-and those gains last. Unlike sleeping pills, CBT-I doesn’t wear off. Medicare started covering CBT-I in 2022, but only 12% of eligible seniors are using it, mostly because providers are scarce.
SSRIs and SNRIs (like sertraline or venlafaxine) are now first-line treatments for chronic anxiety in seniors. They take 4-6 weeks to work, which is slower than a benzodiazepine, but they don’t cause dizziness, memory loss, or falls. They also don’t lead to dependence. And unlike benzodiazepines, they’re safe for long-term use.
Ramelteon is a melatonin receptor agonist approved for sleep onset problems. It’s not a sedative. It doesn’t cause dependency. And it doesn’t impair balance or memory. It’s not perfect-it doesn’t help much with staying asleep-but for seniors who struggle to fall asleep, it’s a solid option.
What about over-the-counter sleep aids? Diphenhydramine (Benadryl) is common, but it’s a big no-no. It has strong anticholinergic effects, which are linked to higher dementia risk. Same goes for hydroxyzine or doxylamine. These aren’t safe just because they’re available without a prescription.
When Might Benzodiazepines Still Be Used?
It’s not all black and white. There are rare cases where benzodiazepines may still be appropriate. For example:
- Short-term use during acute panic attacks
- Severe, treatment-resistant anxiety that hasn’t responded to other therapies
- Procedural sedation before surgery
- End-of-life care for severe distress
Even then, the goal should be to use the lowest possible dose for the shortest possible time. The FDA now requires all benzodiazepine labels to include a warning about dementia risk in seniors, especially for long-acting versions like Valium or Librium.
How to Talk to Your Doctor About Stopping
If you or a loved one has been on benzodiazepines for more than a few months, it’s worth having a conversation. Don’t stop cold turkey. That’s dangerous. Instead, ask:
- “Is this medication still necessary, or was it meant for short-term use?”
- “What are the risks of continuing versus stopping?”
- “Can we try a taper? How long would it take?”
- “Are there non-drug options we can try together?”
Bring the Beers Criteria with you. Print it out. Doctors are more likely to take action when they see evidence-based guidelines. If your provider is hesitant, ask for a referral to a geriatric specialist or a pharmacist trained in deprescribing.
What’s Changing in 2025 and Beyond
Change is happening. Medicare is expanding access to CBT-I. The FDA has updated drug labels. CMS is flagging inappropriate prescriptions in real time. And the American Geriatrics Society has made benzodiazepine deprescribing one of its top priorities for 2025-2027.
There’s even a new NIH-funded trial called BRIGHT, launching in 2024, testing telehealth-assisted tapering for seniors. Results won’t be in until 2029, but the goal is clear: make safe discontinuation easier, faster, and more widely available.
Prescriptions for benzodiazepines in seniors have dropped 18% since 2015. That’s progress. But 3.2 million older adults are still on them. And for those over 85, nearly 1 in 10 are still taking them. That’s too many.
Final Thoughts
Benzodiazepines aren’t evil drugs. They helped many people in the past. But science has moved on. We now know too much about their long-term harm in older adults to keep using them as a first-line fix.
For seniors, the goal isn’t just to manage symptoms-it’s to live safely, clearly, and independently for as long as possible. That means avoiding drugs that cloud the mind, weaken the body, and increase the risk of dementia. Safer alternatives exist. They take time. They require effort. But they’re worth it.
Are benzodiazepines ever safe for elderly patients?
Benzodiazepines can be used in rare, short-term situations-like acute panic attacks, procedural sedation, or end-of-life care. But for chronic anxiety or insomnia, they are not considered safe for older adults. The risks of falls, cognitive decline, and dementia outweigh the benefits. The American Geriatrics Society recommends avoiding them entirely unless no other option exists.
How long does it take to safely stop taking benzodiazepines?
Tapering should be slow and personalized. For most seniors, a 5-10% dose reduction every 1-2 weeks over 8-16 weeks is typical. For those with long-term use, complex health issues, or severe withdrawal symptoms, the process may take 6-12 months. Never stop suddenly. Withdrawal can cause seizures, extreme anxiety, or hallucinations. Always work with a doctor who understands deprescribing.
What are the best non-drug treatments for anxiety and insomnia in seniors?
Cognitive Behavioral Therapy for Insomnia (CBT-I) is the most effective treatment for sleep problems. For anxiety, CBT and mindfulness-based stress reduction show strong results. Physical activity, especially tai chi or gentle yoga, helps reduce both anxiety and improve sleep. Light therapy and regular sleep schedules are also proven tools. These methods don’t carry the side effects of medication and often work better over time.
Can benzodiazepines cause dementia?
Yes, long-term use is strongly linked to increased dementia risk. A 2023 study found seniors who took benzodiazepines for more than six months had an 84% higher risk of developing Alzheimer’s disease. The risk rises with higher doses and longer duration. The FDA now requires all benzodiazepine labels to include a warning about this risk. Even short-term use can have lasting effects on memory and thinking.
Why are benzodiazepines still prescribed if they’re so risky?
Many prescriptions continue because they were started years ago and never re-evaluated. Some doctors aren’t aware of the latest guidelines. Others feel pressured to prescribe because patients ask for them. Also, alternatives like CBT-I aren’t widely available. But awareness is growing. Medicare now covers CBT-I, and providers are being trained to deprescribe. The goal is to stop these prescriptions before they become long-term habits.






