Chronic pain doesn’t just hurt. It wears you down. You stop doing the things you love. You feel guilty for being tired. You start wondering if the pain is all in your head - and that’s when things get worse. You’re not broken. You’re not weak. You’re just stuck in a cycle where pain leads to fear, fear leads to inactivity, and inactivity makes the pain stronger. That’s where CBT for chronic pain comes in. Not as a magic fix, but as a real, research-backed way to take back control.
What CBT for Chronic Pain Actually Does
Cognitive Behavioral Therapy for chronic pain - or CBT-CP - isn’t about pretending your pain isn’t real. It’s about changing how your brain reacts to it. Think of it like upgrading the software on an old phone. The hardware (your body) might still be damaged, but the operating system (your mind) can learn to run more smoothly.
Developed in the 1970s and now used by the U.S. Department of Veterans Affairs and major hospitals nationwide, CBT-CP targets three key problems: pain catastrophizing (thinking the worst), fear-avoidance (stopping movement because you’re scared it’ll hurt), and all-or-nothing thinking (either you’re 100% active or completely bedridden). These patterns don’t cause pain, but they make it worse - and longer-lasting.
A 2023 review of 13 studies with over 1,600 people found that CBT-CP consistently improved mood, sleep, and daily function. For depression and anxiety linked to pain, the benefits were strong. But here’s the truth: it doesn’t always make the pain itself disappear. Only about 25% of studies showed significant pain reduction compared to standard care. That’s not failure. That’s context. CBT-CP isn’t designed to erase pain. It’s designed to help you live with it better.
How It Works: The Core Tools
Most CBT-CP programs last 8 to 16 weeks, with weekly 60- to 90-minute sessions. You don’t need to be a therapist. You just need to show up and try. Here’s what you’ll actually do:
- Pain neuroscience education: You learn how pain works in the nervous system - not just in your back or knee, but in your brain. This isn’t theory. It’s practical. When you understand that pain isn’t always a direct signal of damage, you stop panicking every time you feel a twinge.
- Activity pacing: Instead of pushing through pain until you crash, you learn to break tasks into smaller chunks and schedule rest. One woman in a VA study said, “Learning to pace kept me from my boom-bust cycle.” Boom-bust is when you do too much on a good day, then spend three days in bed recovering. Pacing breaks that cycle.
- Cognitive restructuring: You write down thoughts like “I’ll never get better” or “This pain controls my life,” then challenge them. Not with positive affirmations. With evidence. “Have I had good days before? What did I do differently then?”
- Relaxation and breathing: Chronic pain keeps your nervous system on high alert. Simple breathing exercises and muscle relaxation techniques help turn that down.
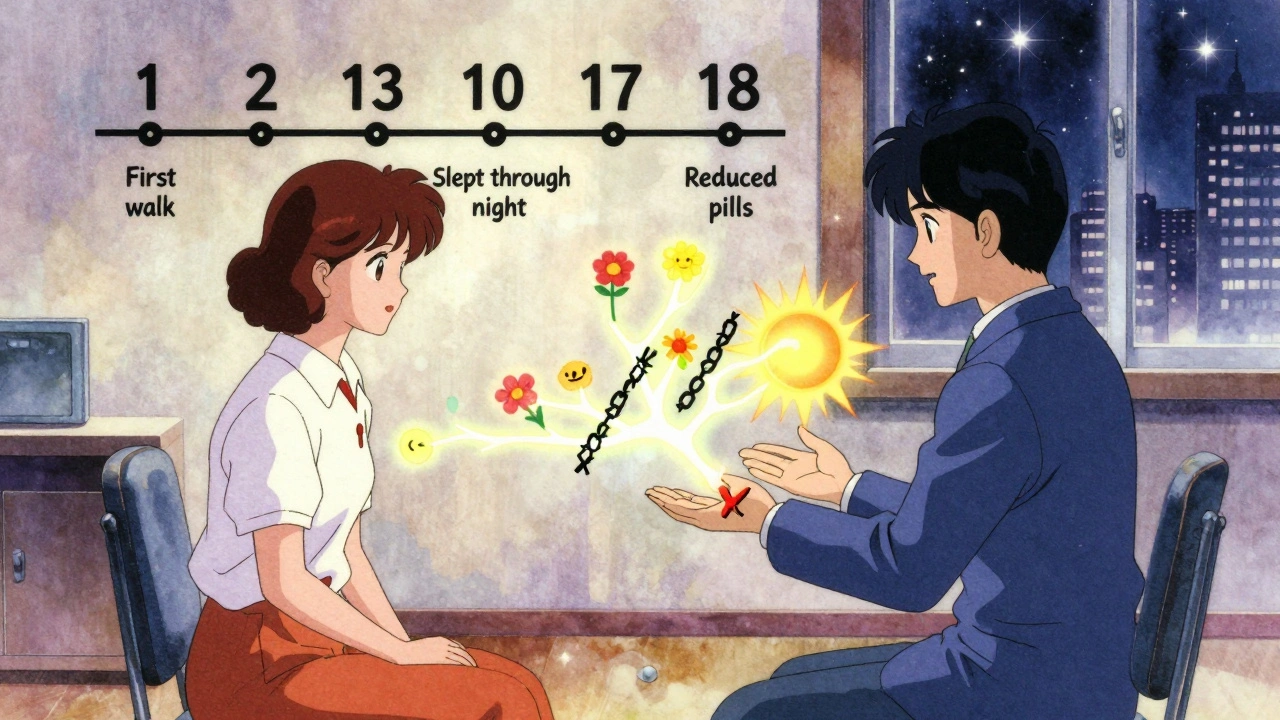
- Behavioral activation: You rebuild activities you’ve given up - even tiny ones. Walking to the mailbox. Cooking one meal. Sitting outside for 10 minutes. Progress isn’t measured in pain scores. It’s measured in moments you didn’t let pain steal.
These aren’t abstract ideas. They’re tools you use daily. One study found people who completed at least 80% of their sessions had 2.3 times higher success rates than those who dropped out.
CBT vs. Other Pain Treatments
Let’s be honest: you’ve probably tried other things. Medications. Physical therapy. Injections. Maybe even opioids. Here’s how CBT-CP stacks up:
| Approach | Effect on Pain Intensity | Effect on Function | Side Effects | Long-Term Sustainability |
|---|---|---|---|---|
| CBT for chronic pain | Moderate to small (d=0.32) | Strong improvement | None | High - skills last |
| Opioids | Moderate (short-term) | Minimal | High - addiction, constipation, tolerance | Low - dependency grows |
| Physical therapy | Moderate | Strong | Low - soreness, fatigue | Moderate - needs ongoing effort |
| Mindfulness therapy | Similar to CBT | Similar to CBT | None | High |
| Acupuncture | Mild to moderate | Mild improvement | Very low | Moderate |
A 2024 trial called STAMP compared CBT-CP directly with mindfulness therapy in 254 people on long-term opioids. At 26 weeks, both worked equally well. But here’s the kicker: 36% of people in the CBT group reduced their daily opioid use. Only 17% did in the control group. That’s not just about pain. That’s about freedom.
CBT-CP doesn’t replace physical therapy. It complements it. People who got both CBT and PT reported 40% greater improvement in daily function than those who got CBT alone. It’s not either/or. It’s both/and.
Who Benefits Most - and Who Might Not
CBT-CP isn’t for everyone. But it works best for certain patterns:
- Best for: People with chronic low back pain, fibromyalgia, or arthritis who also struggle with anxiety, depression, or sleep problems. Women benefit slightly more, and those with college education tend to stick with it longer. If you’ve felt hopeless about your pain, this is your entry point.
- Less effective for: People with pure neuropathic pain (like diabetic nerve pain) or those who are deeply skeptical. If you think “this is all in my head,” you’ll likely drop out. But that’s not a flaw in the therapy - it’s a signal to start with education first.
- Not a quick fix: You won’t feel better after one session. Most people see changes around week 4 to 6. The real gains come between weeks 8 and 12.
One 2023 study even found no significant benefit for men or women in a small group - but that’s an outlier. The overwhelming body of evidence - 37 randomized trials - supports its use. The American Psychological Association gives it a “strong recommendation” for chronic low back pain. That’s the highest level of evidence.
Real People, Real Results
Reddit’s r/ChronicPain community has over 1.2 million members. In 2023-2024, 62% of posts about CBT were positive. Common themes:
- “I stopped avoiding stairs because I learned it wasn’t going to break me.”
- “I cut my pain meds in half after 6 months of CBT.”
- “I finally slept through the night.”
But there’s honesty too. About 29% of negative comments said: “It didn’t fix my pain.” Or “It felt like they were blaming me.” That’s the stigma. CBT isn’t about blaming. It’s about empowering. It’s saying: “Your pain is real. But you’re not powerless.”
One VA patient, a 45-year-old woman with 12 years of back pain, said: “I used to think if I wasn’t 100% active, I was failing. Now I know: showing up for 10 minutes counts.”
How to Get Started
Getting CBT-CP isn’t always easy. Here’s the reality:
- Insurance: Medicare covers only 10 sessions a year - but most programs need 10 to 12. Private insurers vary: UnitedHealthcare covers 12, Aetna covers 8. Check your plan. Ask your doctor to write a letter of medical necessity.
- Access: Only 68% of U.S. commercial insurance plans offer good coverage. Veterans get it easily through the VA. In rural areas, it’s harder. That’s why telehealth is a game-changer. A 2021 study showed video-based CBT worked just as well as in-person.
- Therapists: Look for licensed psychologists or clinical social workers with training in pain psychology. Ask: “Do you use the VA CBT-CP protocol?” or “Are you trained in CBT for chronic pain specifically?”
- Alternatives: If you can’t find a therapist, try FDA-cleared digital CBT apps like PainTrack or CBT-i Coach. They’re not perfect, but they’re better than nothing.
Start by asking your primary care provider: “Can you refer me to someone who does CBT for chronic pain?” If they say no, ask why. Most doctors haven’t been trained in this. That’s changing - slowly.
What to Expect If It Doesn’t Work
Some people try CBT-CP and feel disappointed. Maybe the therapist wasn’t a good fit. Maybe you were in too much pain to focus. Maybe you expected pain to vanish.
That’s okay. It doesn’t mean you failed. It means you tried. And you now know more than most people with chronic pain.
If CBT-CP didn’t click, consider combining it with something else: physical therapy, acupuncture, or even a low-dose antidepressant (which can help pain signals, not just mood). Or try a different therapist. The right fit matters more than the technique.
And if you’re still skeptical? Read the research. Look at the numbers. Over 80% of chronic pain patients are dissatisfied with traditional treatments. CBT-CP isn’t perfect - but it’s one of the few options that doesn’t come with addiction risk, side effects, or a price tag that bankrupts you.
The Bigger Picture
Chronic pain isn’t just a medical problem. It’s a social one. It isolates people. It drains jobs. It breaks families. The healthcare system still treats it like a physical glitch to be fixed - not a whole-person experience to be managed.
CBT-CP is part of a quiet revolution. It’s shifting the focus from “cure the pain” to “restore your life.” It’s not about denying reality. It’s about reclaiming agency.
You don’t need to be pain-free to be whole. CBT-CP helps you live with pain - not as a victim, but as someone who’s still in charge of their choices. Even on the hard days. Especially on the hard days.
Is CBT for chronic pain just talking? Does it really work?
No, it’s not just talking. It’s structured skill-building. You learn specific tools like pacing, thought-challenging, and relaxation - and you practice them daily. Research shows it works: 80% of patients report improved mood and function, and 36% reduce opioid use. It doesn’t erase pain, but it changes how you relate to it.
How long does CBT for chronic pain take to work?
Most people start noticing changes around week 4 to 6. The biggest improvements usually happen between weeks 8 and 12. It’s not instant. But the skills you learn stick around - unlike pills, which stop working when you stop taking them.
Can I do CBT for chronic pain online?
Yes. Video-based CBT (vCBT) has been proven just as effective as in-person sessions. Many insurance plans now cover telehealth CBT. There are also FDA-cleared apps like PainTrack and CBT-i Coach that guide you through core CBT techniques. They’re not a replacement for a therapist, but they’re a great starting point.
Will CBT make me feel like my pain is all in my head?
No. That’s a common misunderstanding. CBT doesn’t say your pain isn’t real. It says your brain’s reaction to pain - fear, avoidance, catastrophizing - can make it worse. It’s about changing your response, not denying your experience. Your pain is real. Your power to respond to it? That’s what CBT helps you reclaim.
Is CBT for chronic pain covered by insurance?
It depends. Medicare covers only 10 sessions per year. Private insurers vary: UnitedHealthcare covers 12, Aetna covers 8. Many plans don’t cover it well - or at all. Ask your provider for a letter of medical necessity. If coverage is poor, look into telehealth options or community health centers that offer sliding-scale fees.
What if I’m on opioids? Can CBT help me reduce them?
Yes. In a major 2024 trial, 36% of patients using CBT reduced their daily opioid use - compared to just 17% in the control group. CBT helps you build confidence in managing pain without relying on medication. It doesn’t force you off opioids. It gives you alternatives so you can choose to reduce them safely.
Do I need a referral to start CBT for chronic pain?
Usually, yes. Most therapists require a referral from a doctor, especially for insurance billing. Start by asking your primary care provider: “Can you refer me to a psychologist who specializes in CBT for chronic pain?” If they say no, ask why - and push for a second opinion. You deserve care that works.







Emily Haworth
December 11, 2025 AT 14:18Tom Zerkoff
December 11, 2025 AT 14:39Deborah Andrich
December 13, 2025 AT 08:20Karen Mccullouch
December 14, 2025 AT 06:48Cole Newman
December 14, 2025 AT 13:06Tyrone Marshall
December 15, 2025 AT 10:01Yatendra S
December 15, 2025 AT 19:12Jamie Clark
December 17, 2025 AT 02:32Donna Hammond
December 18, 2025 AT 17:31nithin Kuntumadugu
December 18, 2025 AT 21:05Harriet Wollaston
December 19, 2025 AT 20:08sharon soila
December 20, 2025 AT 15:21nina nakamura
December 22, 2025 AT 14:11Hamza Laassili
December 23, 2025 AT 06:47Casey Mellish
December 24, 2025 AT 08:40