Warfarin-Estrogen Interaction Calculator
Warfarin & Estrogen Interaction Calculator
Estrogen can significantly affect warfarin effectiveness. Calculate the recommended dose adjustment based on your current INR and estrogen type.
When you're on warfarin, even small changes in your body can throw off your blood thinning. One of the most common but often overlooked triggers? Estrogen. Whether it's birth control pills, hormone replacement therapy, or even some menopause treatments, estrogen can mess with how warfarin works - sometimes making it stronger, sometimes weaker. And that’s dangerous. Too much warfarin means bleeding risk. Too little means clots. Both can kill you.
How Estrogen Changes Warfarin’s Effect
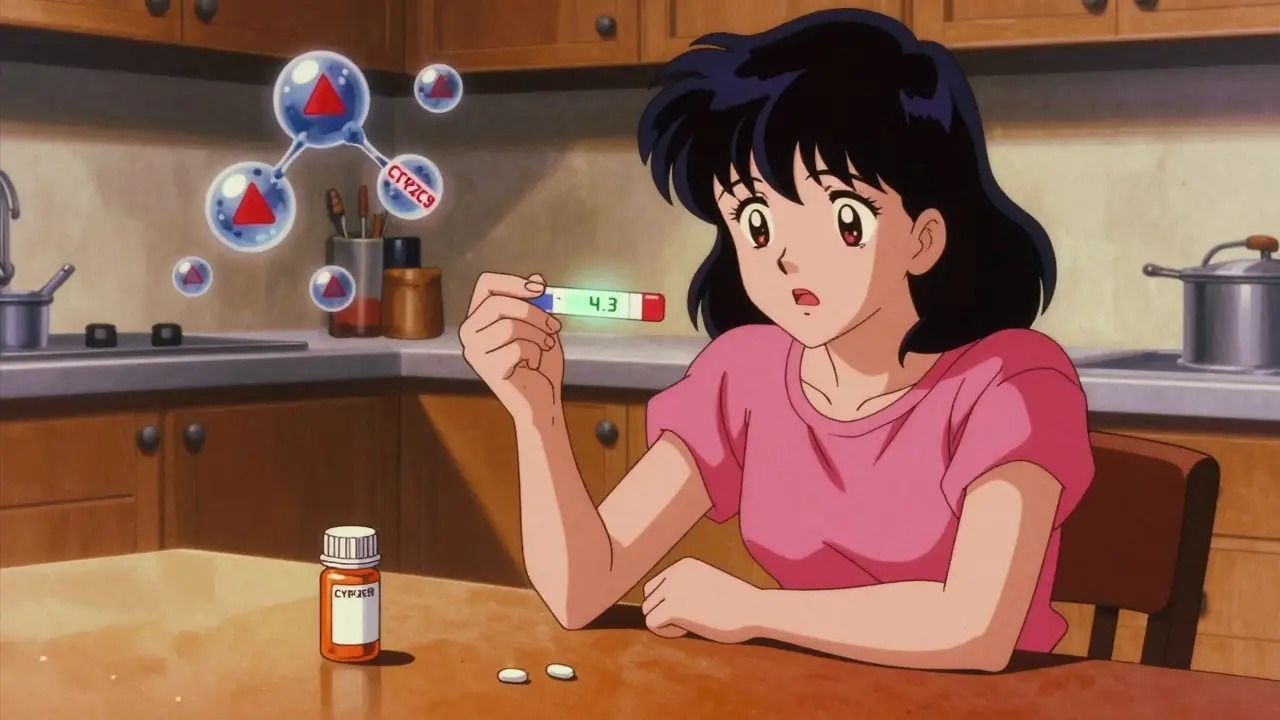
Warfarin doesn’t just float around in your blood doing its job. It’s processed by your liver, mainly by enzymes called CYP450. The most important one for warfarin is CYP2C9, which handles the more powerful part of the drug, S-warfarin. But estrogen compounds - whether natural estradiol or synthetic ethinyl estradiol - don’t play nice with these enzymes. Here’s the twist: not all estrogens act the same. Natural estradiol (used in HRT) tends to induce certain liver enzymes, meaning your body breaks down warfarin faster. That can drop your INR, making warfarin less effective. But synthetic ethinyl estradiol (found in most birth control pills) does the opposite - it inhibits CYP1A2 and CYP2C19, slowing warfarin breakdown. That pushes your INR up, increasing bleeding risk. A 2009 case study in The Annals of Pharmacotherapy showed a 28-year-old woman on warfarin who started a birth control pill. Her INR jumped from 2.4 to 4.3 in just five days. Her warfarin dose had to be cut from 5 mg to 3.5 mg. That’s not rare. The INR Registry tracked over 15,000 patients and found women on estrogen-containing contraceptives were 1.8 times more likely to have INR levels above 4.0 - the danger zone.Why This Isn’t Just About Birth Control
Most people think estrogen interactions only matter for young women on pills. But that’s wrong. Women on hormone therapy after menopause - even those taking low-dose patches or gels - are at risk too. A Reddit user named ClottingSurvivor89 shared: "My INR went from 2.5 to 3.8 within a week of starting HRT. My doctor cut my warfarin by 20%." That’s a real-world example. No lab test, no fancy scan - just a simple blood test and a dose tweak. And it’s not just oral forms. Transdermal estrogen (patches, gels) still gets absorbed into the bloodstream. While some studies suggest they cause fewer interactions than pills, they’re not risk-free. The American College of Chest Physicians says: "All estrogen-containing products require close INR monitoring." No exceptions.How Big Are the Changes? Real Numbers
Not every estrogen interaction causes chaos. Most of the time, INR shifts are modest - between 0.5 and 1.5 units. But with warfarin, even a 0.5-point rise can double your bleeding risk. A 2010 analysis of 15,000+ patients found that estrogen use typically required warfarin dose adjustments of 10-25%. Compare that to other drugs:- Antibiotics like ciprofloxacin: Can spike INR by 2-3 points. Bleeding risk triples.
- SSRIs like fluoxetine: Increase bleeding risk 2.2 times by inhibiting CYP2C9.
- Amiodarone: Requires up to a 40% warfarin dose reduction.
- Estrogen: Usually causes 0.5-1.5 INR changes. Dose adjustment needed in 10-25% of cases.

Genetics Make It Worse (or Better)
Your genes matter. A lot. About 30% of people have a genetic variation in CYP2C9 (like *2 or *3) that slows how fast they break down warfarin. If you’re one of them, even a small estrogen boost can push your INR dangerously high. Another gene, VKORC1, affects how sensitive you are to warfarin. People with the -1639G>A variant need 30-50% less warfarin to stay in range. Combine that with estrogen? You’re playing with fire. The International Warfarin Pharmacogenetics Consortium developed a dosing algorithm that uses your genes + age + weight + meds. It’s 30-35% more accurate than guessing. But only 12% of U.S. clinics test for it. If you’ve been on warfarin for years without a genetic test, you’re flying blind.What Should You Do? Practical Steps
If you’re on warfarin and starting estrogen (or stopping it), here’s what actually works:- Test INR within 3-5 days of starting or stopping estrogen. Don’t wait a week. Don’t wait for symptoms.
- Check again at 7-14 days. Changes can be delayed.
- Adjust dose by 10-25% based on INR trend. If INR rises, reduce warfarin. If it drops, increase it.
- Don’t assume" it’s just diet". Vitamin K changes are common - but so are estrogen effects. Rule out estrogen first if you’re on it.
- Talk to your pharmacist. They see these interactions daily. 68% of pharmacists report managing at least one estrogen-warfarin case per year.

Why DOACs Are Changing the Game
Direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, and dabigatran don’t rely on CYP enzymes the same way warfarin does. They’re less affected by estrogen. That’s why DOAC prescriptions jumped from 15% of all oral anticoagulant use in 2013 to 68% in 2022. But DOACs aren’t for everyone. People with mechanical heart valves, severe kidney disease, or antiphospholipid syndrome still need warfarin. The American College of Cardiology says 1.8 million Americans will still be on warfarin in 2030. That means this interaction isn’t going away.What No One Tells You
The biggest problem? Confusion. A patient might have an elevated INR and blame it on eating too much kale. Or a doctor might think it’s a "random fluctuation." But if you’re on estrogen, that’s the first thing to check. And if you’re on warfarin and your doctor says "hormones don’t matter," they’re outdated. The FDA updated warfarin labeling in January 2023 to include clearer warnings about estrogen interactions. That’s progress. But it’s still up to you - and your care team - to connect the dots.Final Takeaway
Estrogen and warfarin don’t always cause big problems. But when they do, it’s sudden, silent, and serious. You don’t need to stop estrogen. You don’t need to stop warfarin. You just need to know the risk, monitor closely, and adjust early. One simple blood test, done at the right time, can prevent a trip to the ER.Can birth control pills really affect my warfarin?
Yes. Synthetic estrogen in birth control pills can inhibit liver enzymes that break down warfarin, causing your INR to rise. Studies show women on these pills are nearly twice as likely to have INR levels above 4.0 - the danger zone for bleeding. Always check your INR within 3-5 days of starting or stopping birth control.
Does hormone replacement therapy (HRT) interact with warfarin?
Yes. Even topical estrogen patches or gels can affect warfarin. Natural estradiol may lower warfarin levels by speeding up its metabolism, while some formulations can still cause INR spikes. The American College of Chest Physicians recommends monitoring INR within 3-5 days of starting or stopping any estrogen therapy, regardless of delivery method.
How long does it take for estrogen to affect my INR?
It varies. Some people see changes in 2-3 days; others take 7-10 days. That’s why guidelines recommend checking INR at day 3-5, then again at 7-14 days. Don’t wait for symptoms like bruising or nosebleeds - by then, it’s already too late.
Should I switch from warfarin to a DOAC if I’m on estrogen?
Maybe. DOACs have fewer drug interactions with estrogen and don’t require frequent blood tests. But they’re not safe for everyone - especially if you have mechanical heart valves, severe kidney disease, or antiphospholipid syndrome. Talk to your hematologist. Don’t switch on your own.
Can genetic testing help me manage this interaction?
Yes. If you have CYP2C9*2, *3, or VKORC1 -1639G>A variants, you’re more sensitive to warfarin and more vulnerable to estrogen interactions. Genetic testing improves dosing accuracy by 30-35%. While not routine yet, ask your doctor if you’ve had unstable INRs or multiple dose changes.
What if my INR goes down when I start estrogen?
That can happen too. Natural estradiol (used in HRT) may induce liver enzymes, causing your body to clear warfarin faster. If your INR drops below your target, your dose may need to be increased. This is less common than INR spikes, but still documented in clinical studies. Always monitor - don’t assume it’s "safe" just because your INR didn’t go up.






Linda Franchock
February 16, 2026 AT 18:28