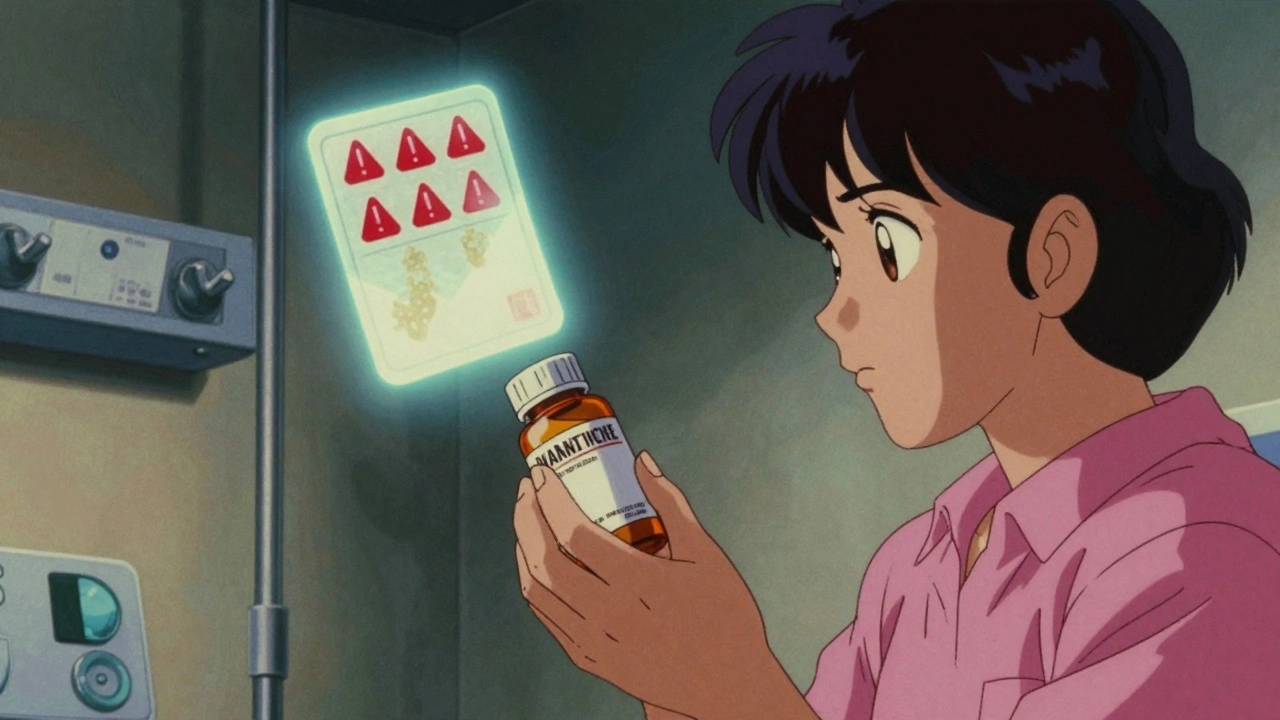
Every year, millions of Americans take generic drugs because they’re cheaper, just as effective, and approved by the FDA. But here’s something most people don’t realize: the safety warnings on your generic pill might be outdated, even if the brand-name version has been updated with new risks. This isn’t a glitch. It’s how the system was designed.
Why Generic Drug Warnings Lag Behind
In 1984, Congress passed the Hatch-Waxman Act to speed up access to affordable medicines. It worked-today, generics make up over 90% of prescriptions filled in the U.S. But there was a trade-off. The law required generic manufacturers to copy the exact label of the original brand-name drug. That includes warnings about side effects, drug interactions, and black box alerts. If the brand-name company adds a new warning, the generic maker can’t update its label unless the FDA approves the change. That approval process can take months. Meanwhile, patients on the generic version keep taking the drug with old, incomplete safety info. A 2013 FDA proposal tried to fix this by letting generic manufacturers use the same quick-update tool as brand-name companies: the Changes Being Effected (CBE-0) process. That tool lets drugmakers add new safety info without waiting for FDA approval. But it’s still only available to brand-name makers.Who’s Affected-and How
If you’re on a generic drug, you’re likely getting the same active ingredient as the brand version. But you might not get the same safety updates. Take a common example: a blood thinner. If the brand-name version adds a warning about increased bleeding risk in elderly patients, the generic version stays the same until the FDA acts. That delay could mean a senior patient on the generic doesn’t know to watch for bruising or dizziness. This isn’t theoretical. In 2022, 27 consumer health groups wrote to the FDA, arguing that patients deserve equal access to safety information. “Many insurance companies require patients to take a generic drug if it is available,” they pointed out. “Those patients deserve quality, updated information on the drugs they take.” The generic drug industry pushes back. They say forcing them to change labels unilaterally opens them up to lawsuits. If a patient has a bad reaction after a label update, who’s liable-the generic maker who added the warning, or the brand maker who didn’t update it fast enough? Legal experts say this is a minefield. Brand-name companies are already sued regularly for delayed warnings. Adding that risk to generics could scare manufacturers out of the market, reducing competition and driving prices up.How the FDA Monitors Generic Drug Safety
The FDA doesn’t just sit back and wait for problems. Its MedWatch program collects over 100,000 adverse event reports every year-from doctors, pharmacists, and even patients. The FDA’s Office of Generic Drugs runs monthly checks on the FDA Adverse Event Reporting System (FAERS) to spot patterns. In 2019, when the first generic version of the antipsychotic Rexulti hit the market, the FDA monitored it closely for a full year. No safety signals showed up. That’s good news. But not all generics are simple. Complex ones-like extended-release injectables, transdermal patches, or eye drops-can behave differently even with the same active ingredient. That’s because of differences in excipients: the inactive ingredients like preservatives, dyes, or thickening agents. The FDA requires identical excipients in some cases, like ophthalmic and injectable generics. But for others, small changes can affect how the drug is absorbed. Dr. Xin Fu, who leads excipient safety assessments at the FDA, says these differences “may change the safety profile” depending on how long someone takes the drug or what other meds they’re on.
What You Can Do Right Now
You don’t have to wait for the FDA to fix this. Here’s what you can do:- Check the FDA’s Drug Safety and Availability page regularly. It lists all recent alerts, including for generics.
- Ask your pharmacist: “Is this generic version updated with the latest safety warnings?” They have access to the same label databases as the FDA.
- Sign up for MedWatch alerts. You can report side effects yourself-and get email updates when new warnings come out.
- If you’re on a generic drug with known risks (like blood thinners, seizure meds, or psychiatric drugs), keep a symptom journal. Note any new dizziness, rashes, or mood changes.
The Bigger Picture: Cost vs. Safety
Generic drugs saved U.S. patients over $300 billion in 2023 alone. That’s huge. But safety isn’t a luxury-it’s a baseline. The current system forces patients to choose between affordability and timely information. And for many, the choice isn’t even theirs-insurance plans mandate generics. The FDA’s 2013 proposal to let generics update labels independently is still pending. No final rule has been issued as of late 2024. Until then, the gap remains. Some experts say the solution isn’t to force generics to carry full liability, but to create a shared responsibility model. Maybe the brand-name maker should be required to notify all generic makers of new safety data within 30 days. Maybe the FDA should publish a centralized, real-time alert feed for all versions of a drug-brand and generic alike.
What’s Next?
The number of complex generics is rising. More injectables, more patches, more long-acting forms. These aren’t just pills you swallow-they’re engineered systems. And their safety profiles are harder to predict. The FDA is already shifting resources to monitor these products more closely. Meanwhile, patients are catching on. Online forums are buzzing about label discrepancies. A Reddit thread in October 2024 had over 2,000 comments from people who noticed their generic blood pressure pill didn’t mention the same dizziness warning as the brand version. One woman wrote: “I switched back to the brand because I didn’t feel safe taking something with outdated info.” This isn’t about distrust in generics. It’s about transparency. The FDA approves them as safe and effective. That’s not in question. But safety warnings? Those need to keep pace.Are generic drugs less safe than brand-name drugs?
No. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and performance as the brand-name version. They’re tested to ensure they work the same way in your body. The difference isn’t safety or effectiveness-it’s the timeliness of safety warnings on the label.
Can I trust the safety information on a generic drug label?
You can trust that the information is accurate as of the last FDA-approved update. But if the brand-name version added a new warning six months ago, your generic may still show the old version. Always check the FDA’s Drug Safety and Availability page for the latest alerts, regardless of which version you’re taking.
Why can’t generic manufacturers update their own labels?
Current FDA rules require generic manufacturers to mirror the brand-name label exactly. Only the original manufacturer can use the quick-update process (CBE-0) to add new safety info without waiting for FDA approval. A 2013 proposal would change this, but it’s still under review as of 2024.
How do I find out if my generic drug has a new safety alert?
Go to the FDA’s Drug Safety and Availability page and search for your drug’s name. You’ll see all recent alerts, whether for brand or generic versions. You can also sign up for MedWatch email alerts. Your pharmacist can also check the FDA’s current labeling database for you.
Should I switch from a generic to a brand-name drug for safety reasons?
Only if your doctor recommends it. Most generics are perfectly safe. But if you’re taking a high-risk medication-like an anticoagulant, seizure drug, or psychiatric medication-and you’ve noticed new side effects, it’s worth asking your doctor if the label on your generic is up to date. Sometimes, the brand version is worth the extra cost for peace of mind.






Ignacio Pacheco
December 2, 2025 AT 14:18Makenzie Keely
December 3, 2025 AT 09:43Chloe Madison
December 3, 2025 AT 11:47Vincent Soldja
December 5, 2025 AT 01:41Myson Jones
December 5, 2025 AT 11:12Joykrishna Banerjee
December 5, 2025 AT 13:10Kidar Saleh
December 6, 2025 AT 17:10Archie singh
December 7, 2025 AT 00:00Gene Linetsky
December 8, 2025 AT 05:42Katherine Gianelli
December 9, 2025 AT 00:09Francine Phillips
December 10, 2025 AT 19:31Jim Schultz
December 12, 2025 AT 10:59