Obesity isn’t just about eating too much or not exercising enough. It’s a chronic disease - one that affects your heart, your blood sugar, your joints, and even your mood. And like high blood pressure or diabetes, it needs ongoing medical care. That’s where medical weight management comes in. This isn’t another diet plan you’ll quit after a month. It’s a structured, science-backed system that combines doctor oversight, prescription medications, nutrition coaching, and regular monitoring to help you lose weight and keep it off - safely and sustainably.
What Medical Weight Management Actually Looks Like
Most people think weight loss means counting calories or buying shakes. But medical weight management is different. It starts with a clear diagnosis. If your BMI is 30 or higher, or 27 or higher with conditions like high blood pressure, prediabetes, or sleep apnea, you’re eligible. That’s not a suggestion - it’s the standard set by the American College of Cardiology’s 2025 guidelines. From there, you enter a clinic-based program. These aren’t just doctor’s offices with a scale. They’re multidisciplinary teams: physicians trained in obesity medicine, registered dietitians, behavioral health coaches, and sometimes even exercise physiologists. You don’t just get a prescription. You get a plan tailored to your life. One patient might need help managing stress eating. Another might need to adjust their insulin while losing weight. The plan changes as you change. West Virginia University’s program, for example, requires patients to complete a pre-recorded orientation and fill out detailed questionnaires before their first visit. Why? Because they know that understanding your triggers - whether it’s late-night snacking, emotional eating, or lack of sleep - is half the battle. Their patient handbook covers everything from portion control to walking routines. No guesswork. No confusion.The Medications: More Than Just a Trend
You’ve seen the ads. Semaglutide. Tirzepatide. These aren’t new fads. They’re GLP-1 receptor agonists - drugs originally developed for type 2 diabetes that turned out to be incredibly effective for weight loss. And the data is undeniable. In clinical trials, semaglutide (Wegovy®) helped people lose an average of 14.9% of their body weight over 72 weeks. Tirzepatide (Zepbound®), a newer dual-action drug, pushed that to 20.2%. That’s not a few pounds. That’s real, measurable improvement in blood pressure, cholesterol, and insulin sensitivity. And for people with type 2 diabetes, losing 10% or more of body weight can actually put the disease into remission - something the American Diabetes Association now calls a primary treatment goal. There’s even a new triple agonist, retatrutide, showing 24.2% weight loss in early trials. But here’s the catch: these medications aren’t magic pills. They work best when paired with nutrition and behavior change. And they’re expensive. Insurance covers them for only 68% of commercially insured patients. Medicare Advantage plans cover them for just 12%. Many people wait months just to get approval.Monitoring: Why Tracking Matters More Than You Think
You wouldn’t manage high blood pressure without checking your numbers. Why treat obesity any differently? The American Diabetes Association recommends measuring weight, waist circumference, and blood pressure at least every three months during active treatment. That’s not just for the doctor’s records - it’s for you. Seeing progress - even if it’s slow - keeps you motivated. A 2024 JAMA Internal Medicine study found that people in medically supervised programs lost nearly twice as much weight (9.2%) as those in commercial programs (5.1%) over 12 months. Why? Because they were monitored. Someone was checking in. Someone noticed if weight loss stalled. Someone adjusted the plan. Many clinics now use digital tools. The MyWVUChart app, for example, asks patients weekly questions about sleep, mood, hunger, and activity. It flags patterns - like “you lost 3 pounds last week but gained 2 back after a stressful work week.” That’s not surveillance. That’s insight. And it’s not just about the scale. Waist circumference matters more than weight for predicting heart disease risk. Blood tests for liver enzymes, HbA1c, and lipids are tracked over time. These numbers tell the real story of whether your health is improving - not just whether you’re lighter.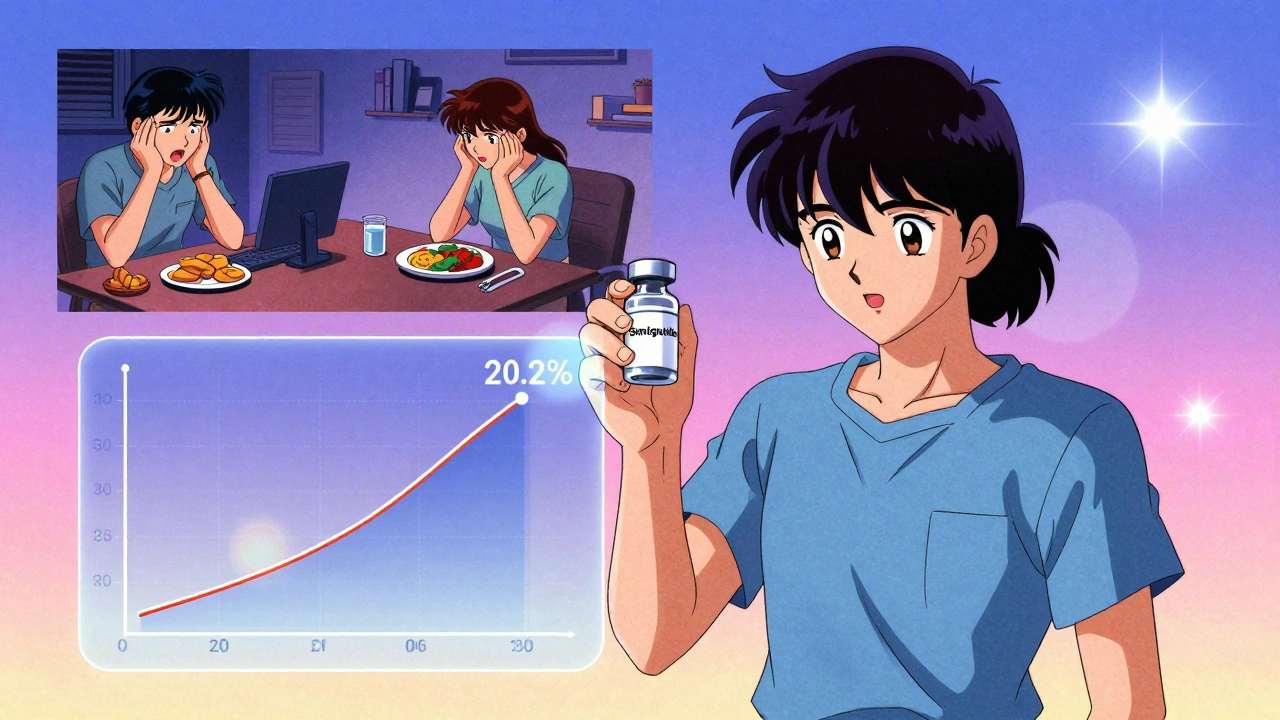
Clinics vs. Commercial Programs: The Real Difference
You can buy a weight loss program online for $30 a month. Or you can join a medical clinic for $200-$300. Which is worth it? The numbers don’t lie. Medical programs deliver better results. But they also cost more. Why? Because they’re staffed by licensed professionals who adjust treatment based on your biology, not your motivation. Commercial programs often rely on generic meal plans and group calls. Medical clinics use personalized nutrition therapy - 45- to 60-minute sessions with a dietitian who understands how your body responds to carbs, protein, and fat. One patient told Reddit: “I tried Weight Watchers for a year. Lost 12 pounds. Gained back 20. Then I went to the university clinic. Lost 40 pounds in 8 months. My A1c dropped from 6.8 to 5.4.” The difference? Medical weight management treats you as a patient, not a customer. It’s not about selling a product. It’s about managing a disease.Barriers Nobody Talks About
Let’s be honest: access isn’t equal. Black and Hispanic patients are 43% less likely to be offered weight-loss medications - even when they meet the same BMI and health criteria as white patients. That’s not an accident. It’s systemic bias. Insurance denial is another silent roadblock. One patient waited six weeks just to get approval for semaglutide. Another was told, “You’re not sick enough.” That’s not medical advice - that’s stigma. Clinics are working to fix this. The ACC’s 2025 guidelines urge providers to use chairs without armrests, offer blood pressure cuffs in multiple sizes, and avoid phrases like “you need to try harder.” Language matters. Environment matters. Respect matters.Who Benefits Most?
Medical weight management isn’t just for people with BMI 40+. It’s for anyone with obesity-related health problems. That includes:- People with prediabetes or type 2 diabetes
- Those with high blood pressure or high cholesterol
- Individuals with sleep apnea or fatty liver disease
- People who’ve tried diets and kept regaining weight
The Future Is Here - And It’s Personalized
By 2030, the American Diabetes Association predicts weight management will be as routine in diabetes care as checking HbA1c. That’s not hype. It’s science. Forty-seven percent of Fortune 500 companies now offer medical weight management as part of employee wellness programs. That’s up from 18% in 2022. Why? Because every dollar invested in these programs returns $2.87 in reduced healthcare costs for diabetes and heart disease within five years. The field is growing fast. In 2025, 92% of U.S. medical schools teach obesity medicine - up from 36% in 2015. More doctors are getting certified. More clinics are opening. More patients are finding relief. This isn’t about being thin. It’s about being healthy. About lowering your risk of a heart attack. About sleeping better. About feeling stronger. About living longer.Frequently Asked Questions
Is medical weight management only for people with severe obesity?
No. Medical weight management is for anyone with a BMI of 30 or higher, or a BMI of 27 or higher with at least one obesity-related condition like high blood pressure, prediabetes, or sleep apnea. You don’t need to be severely obese to qualify. In fact, early intervention often leads to better long-term results and can prevent more serious health problems down the road.
Are weight-loss medications like Wegovy and Zepbound safe?
Yes, when used under medical supervision. These medications have been studied in tens of thousands of patients over years. Common side effects include nausea, constipation, or mild stomach discomfort - usually temporary. Serious side effects are rare. The risk of complications from these medications is about 0.2%, compared to 4.7% for bariatric surgery. They’re not for everyone, but for many, the benefits far outweigh the risks.
How long do I need to stay on medication?
Obesity is a chronic condition, so treatment is often long-term - similar to taking blood pressure or cholesterol medication. Stopping the medication usually leads to weight regain. But that doesn’t mean you’ll be on it forever. Some people work with their provider to reduce dosage over time as they build sustainable habits. Others continue indefinitely. The goal isn’t lifelong dependence - it’s lifelong health.
What if my insurance doesn’t cover these medications?
Insurance coverage is still inconsistent. Only 68% of commercial plans cover anti-obesity meds, and Medicare Advantage plans cover them for just 12%. If you’re denied, ask your clinic for help - many have patient assistance programs, manufacturer coupons, or payment plans. Some clinics also offer sliding-scale fees based on income. Don’t give up. Ask for alternatives. Sometimes, starting with nutrition and behavior therapy alone can help you qualify for coverage later.
Can I do this without seeing a doctor?
You can lose weight on your own - but keeping it off is much harder. Medical weight management works because it’s not just about food and exercise. It’s about understanding your biology, your habits, your mental health, and your environment. A doctor can rule out thyroid issues, adjust medications that cause weight gain, and prescribe drugs that help your body stop fighting weight loss. You can’t do all that alone.






Jane Quitain
December 6, 2025 AT 23:55Sam Mathew Cheriyan
December 8, 2025 AT 18:05Ernie Blevins
December 10, 2025 AT 12:15David Brooks
December 10, 2025 AT 14:19Sadie Nastor
December 10, 2025 AT 19:07Stacy here
December 11, 2025 AT 11:37Kyle Flores
December 13, 2025 AT 05:31Olivia Hand
December 14, 2025 AT 08:29Desmond Khoo
December 14, 2025 AT 20:22Louis Llaine
December 15, 2025 AT 11:10Kurt Russell
December 17, 2025 AT 08:53Ryan Sullivan
December 18, 2025 AT 18:43Helen Maples
December 19, 2025 AT 03:45Jennifer Anderson
December 20, 2025 AT 09:09Sangram Lavte
December 21, 2025 AT 11:29