SGLT2 Inhibitor Risk Assessment Tool
Assess Your Risk
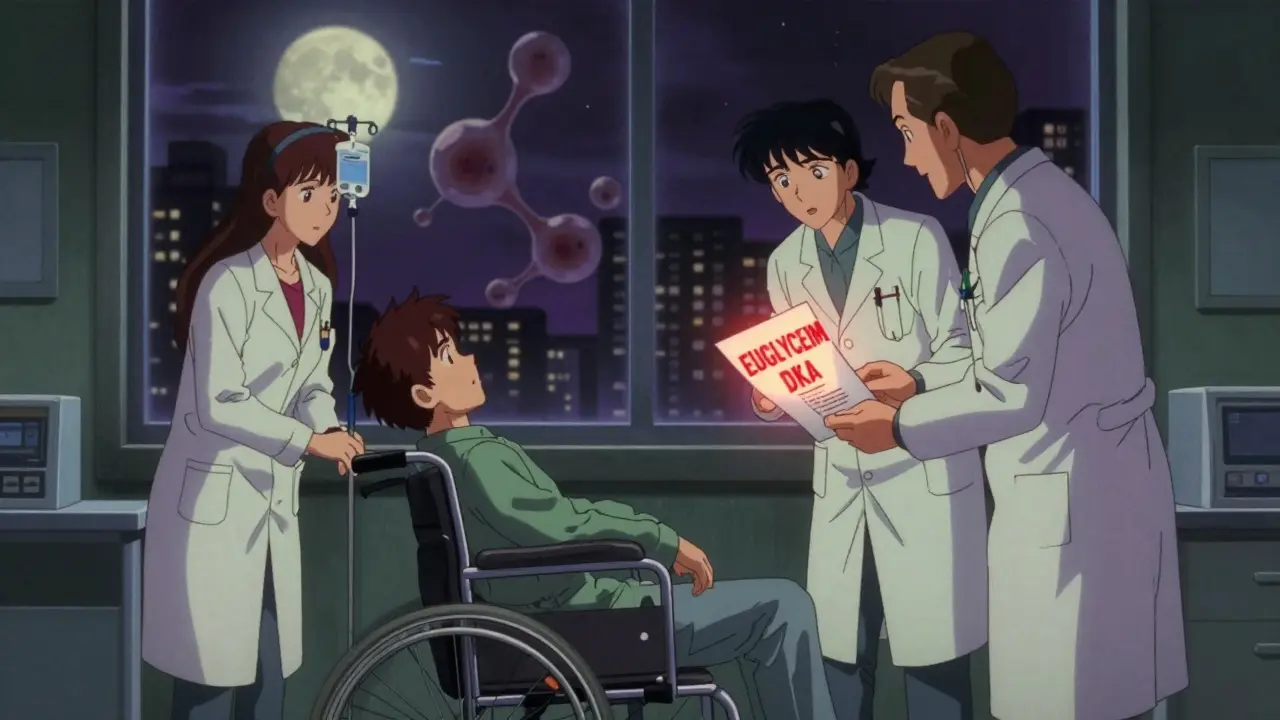
This tool evaluates your risk of developing euglycemic diabetic ketoacidosis (euDKA) while taking SGLT2 inhibitors. Based on your answers, it will show your risk level and specific recommendations.
Risk Assessment Result
When you hear about SGLT2 inhibitors, you might think of weight loss, better heart health, or kidney protection. And for many people with type 2 diabetes, those benefits are real. But there’s a quiet, dangerous side effect that doesn’t get talked about enough: diabetic ketoacidosis - and not the kind you expect.
What You Don’t Know About DKA Can Kill You
Most people think diabetic ketoacidosis (DKA) means blood sugar over 250 mg/dL, vomiting, fruity breath, and confusion. That’s the classic version. But with SGLT2 inhibitors, the story changes. A growing number of cases show up with blood sugar levels under 200 mg/dL - sometimes even normal. This is called euglycemic DKA, or euDKA. And it’s sneaky.Because the numbers look okay, patients and even doctors miss it. A 2023 FDA analysis found nearly half of all DKA cases linked to SGLT2 inhibitors had blood glucose below 250 mg/dL. People showed up with nausea, fatigue, abdominal pain, or trouble breathing - symptoms that look like the flu or food poisoning. By the time ketones are checked, it’s already an emergency.
Here’s the hard truth: euDKA isn’t rare. Studies show it happens 2 to 3 times more often with SGLT2 inhibitors than with other diabetes meds like DPP-4 inhibitors. The European Medicines Agency confirmed this in 2023, updating safety labels to warn doctors: “Check for ketoacidosis even if blood sugar isn’t high.”
How SGLT2 Inhibitors Trigger This Risk
SGLT2 inhibitors - like canagliflozin, dapagliflozin, empagliflozin, and ertugliflozin - work by making your kidneys dump sugar into your urine. That lowers blood sugar. But here’s the catch: they also lower insulin slightly and increase glucagon. That pushes your body to burn fat for fuel instead of glucose.That sounds fine - until you’re sick, fasting, or cutting carbs. Suddenly, your body is flooded with ketones. Normally, insulin would shut that down. But with SGLT2 inhibitors, insulin is already suppressed. And if you’re on low insulin (like if you have type 2 diabetes with beta-cell decline), your body has no brakes.
It’s not just the drug. It’s what happens around it. The biggest triggers? Illness (like a cold or flu), surgery, skipping meals, drinking too much alcohol, or cutting your insulin dose. One study found 33% of euDKA cases happened during illness. Another 24% followed insulin reduction.
Who’s Most at Risk?
Not everyone on SGLT2 inhibitors gets euDKA. But some people are far more vulnerable.- People with low C-peptide - this means your pancreas isn’t making much insulin anymore. If your C-peptide is below 1.0 ng/mL, your risk jumps to over 2% - compared to less than 1% in those with normal insulin production.
- People with type 1 diabetes - even though these drugs aren’t approved for type 1, some doctors prescribe them off-label. The FDA and ADA warn against this unless under strict supervision.
- Those planning surgery - fasting before surgery can trigger euDKA. Guidelines now say stop SGLT2 inhibitors at least 3 days before any procedure.
- People on high doses - canagliflozin 300 mg carries more risk than 100 mg.
- Those with recent weight loss or low-carb diets - if you’re eating fewer carbs, your body is already primed to burn fat. SGLT2 inhibitors push you over the edge.
One study tracked 1,247 DKA cases linked to these drugs. Over 60% happened within the first year. The average time to onset? Just 28 weeks after starting the pill.
What Doctors Should Do - And What You Should Ask
The American Diabetes Association, the Endocrine Society, and the American Association of Clinical Endocrinologists all agree: education saves lives.Doctors need to screen before prescribing. Ask: Have you ever had DKA? Do you have signs of insulin deficiency? Are you planning surgery? Are you on a low-carb diet? If any of these are yes, SGLT2 inhibitors might not be the right choice.
And if you’re already on one? You need to know the warning signs: nausea, vomiting, stomach pain, tiredness, trouble breathing, confusion. Don’t wait for high blood sugar. If you feel off - check ketones. Use a urine strip or a blood ketone meter. If ketones are moderate or high, go to the ER. Don’t wait. Don’t try to tough it out.
A 2022 study showed that when patients were taught to check ketones when sick, DKA cases dropped by 67%. That’s not a small win. That’s life-saving.
Why the Debate Still Exists
You might read conflicting studies. Some say SGLT2 inhibitors don’t raise DKA risk. Others say they triple it. What’s going on?It comes down to who’s being studied. Trials with healthy, insulin-producing type 2 patients show low risk. Real-world data - where people are older, sicker, on less insulin, and eating poorly - shows higher risk. One 2023 meta-analysis of 71,000 people found no difference from placebo. But that was mostly in controlled trials. The real-world data from Canada and the UK, tracking over 350,000 people, showed a 2.85 times higher risk.
And then there’s the type 1 diabetes angle. A 2025 analysis found no increased risk in type 1 patients using SGLT2 inhibitors - but only when insulin was carefully adjusted. That’s not a green light. It’s a warning: only under expert care.

The Bottom Line: Benefits vs. Risk
Let’s be clear: SGLT2 inhibitors work. They cut heart attacks, hospitalizations for heart failure, and kidney decline. In landmark trials like EMPA-REG and DECLARE-TIMI, they saved lives. For many, the benefits outweigh the risk.But risk isn’t zero. And it’s not evenly distributed. For someone with strong insulin production, no history of DKA, and no planned surgery - the risk is low. For someone with declining beta-cell function, a recent infection, and a low-carb diet? The risk is real. And deadly.
The key isn’t avoiding these drugs altogether. It’s knowing who they’re safe for - and who they’re not. It’s asking the right questions. It’s checking ketones when you’re sick. It’s stopping the pill before surgery. It’s listening to your body when something feels off.
These drugs aren’t magic. They’re powerful tools. And like any tool, they can hurt you if you don’t use them wisely.
What to Do Right Now
If you’re on an SGLT2 inhibitor:- Know the symptoms of DKA - nausea, vomiting, stomach pain, fatigue, trouble breathing.
- Get a ketone test strip or meter. Keep it at home.
- Check ketones if you’re sick, fasting, or stressed - even if your blood sugar is normal.
- Stop the drug 3 days before any surgery or medical procedure.
- Talk to your doctor: Is your insulin production still strong? Are you a good candidate to keep taking this?
If you’re considering starting one:
- Ask for a C-peptide test. It tells you how much insulin your body still makes.
- Discuss your diet. Are you cutting carbs? That’s a red flag.
- Ask: What’s my history with DKA? Have I ever had unexplained nausea or vomiting?
- Don’t let the weight loss or heart benefits blind you to the hidden danger.
Can SGLT2 inhibitors cause DKA even if my blood sugar is normal?
Yes. This is called euglycemic DKA, and it’s a known risk with SGLT2 inhibitors. Blood sugar can be under 200 mg/dL - sometimes even normal - while ketones rise to dangerous levels. Symptoms like nausea, vomiting, fatigue, and trouble breathing can appear without high blood sugar, making it easy to miss.
How common is DKA with SGLT2 inhibitors?
The risk is low overall - about 0.1 to 0.5 cases per 100 patients per year. But it’s 2 to 3 times higher than with other diabetes medications like DPP-4 inhibitors. Most cases happen within the first year, often triggered by illness, surgery, or low-carb diets.
Should I stop taking my SGLT2 inhibitor if I get sick?
Yes - temporarily. If you’re sick with an infection, vomiting, or unable to eat, stop your SGLT2 inhibitor and check ketones. Contact your doctor. Do not restart until you’re fully recovered and eating normally. Guidelines recommend stopping at least 3 days before any surgery or medical procedure.
Are SGLT2 inhibitors safe for type 1 diabetes?
No - not without strict supervision. While some studies show they can be used in type 1 diabetes under close care, they’re not FDA-approved for this use. The risk of euDKA is significantly higher in people with little or no insulin production. Most guidelines strongly advise against using them in type 1 diabetes unless part of a controlled, expert-managed program.
What should I do if my ketone test is positive?
If your ketones are moderate or large - even if your blood sugar is normal - go to the emergency room immediately. Do not wait. Do not try to treat it at home. euDKA can worsen quickly and is life-threatening. Bring your medication list and tell them you’re on an SGLT2 inhibitor.
Is there a way to reduce my risk of euDKA?
Yes. Stay hydrated, avoid low-carb diets unless under medical supervision, check ketones when you’re sick, and stop the drug before surgery. Ask your doctor for a C-peptide test to see how much insulin your body still makes. If your C-peptide is low, you’re at higher risk - and may need to reconsider this medication.







Randolph Rickman
December 16, 2025 AT 07:07Man, I was on empagliflozin for a year and never knew this was a thing. I got really sick last winter with what I thought was the flu-nausea, no appetite, just wiped out. Turns out my ketones were through the roof. My doc didn’t even think to check until I insisted. This post saved my life. If you’re on one of these drugs, get a ketone strip. Seriously. Keep one in your bathroom drawer. It’s that simple.
Mike Smith
December 18, 2025 AT 00:46Thank you for sharing this critical information with such clarity and care. As a healthcare provider, I’ve seen too many patients dismissed because their glucose levels were ‘not high enough.’ Euglycemic DKA is a silent killer, and awareness is the first line of defense. I now routinely screen for C-peptide and educate patients on ketone monitoring-especially before procedures or during illness. Knowledge truly is power, and this post empowers both clinicians and patients.
Aditya Kumar
December 19, 2025 AT 16:48Whatever.
Colleen Bigelow
December 21, 2025 AT 09:59Big Pharma doesn’t want you to know this. They make billions off these drugs while quietly burying the data. The FDA? Compromised. Doctors? Brainwashed by reps with free lunches. I’ve seen it happen-people get put on these pills for weight loss, then end up in the ER with acidosis and no one connects the dots. It’s not an accident. It’s a cover-up. And they’re doing it to you too. Check your meds. Check your labels. Don’t trust the system.
Billy Poling
December 23, 2025 AT 01:28While I appreciate the intent behind this post, I must express my concern regarding the lack of precise statistical context and the potential for misinterpretation by laypersons. The absolute risk of euglycemic DKA remains statistically low, even with SGLT2 inhibitors, and the relative risk increase must be contextualized within the broader cardiovascular and renal benefits demonstrated in multiple large-scale, randomized controlled trials. Moreover, the distinction between type 1 and type 2 diabetes in terms of beta-cell function is not always clinically evident without formal testing, which may lead to unnecessary discontinuation of beneficial therapy in appropriate candidates. A balanced risk-benefit analysis, guided by individualized clinical assessment, remains paramount.
Elizabeth Bauman
December 23, 2025 AT 20:57Y’all are sleeping on this. Big Pharma is pushing these drugs like they’re candy. They don’t care if you die-they care if you keep buying. I got a letter from my insurance company last month saying they’re dropping metformin coverage and pushing SGLT2 inhibitors instead. Coincidence? Nah. They’re gambling with your life for profit. If you’re on one of these, stop. Talk to your doctor. Demand a C-peptide test. Don’t let them gaslight you with ‘your numbers are fine.’
Dylan Smith
December 25, 2025 AT 03:41I’ve been on dapagliflozin for 8 months and lost 20 lbs. I feel great. But now I’m scared. I had that weird stomach pain last week and thought it was just indigestion. Should I have checked ketones? I didn’t even know I could. I’m getting strips today. And I’m asking my doc about my C-peptide. This post scared me but also woke me up. Thanks.
Ron Williams
December 25, 2025 AT 09:35As someone who’s lived with type 2 for 15 years, I’ve seen a lot of trends come and go. This one’s real. I had a friend who got euDKA after a weekend camping trip-he skipped meals, drank a few beers, and thought he was fine because his glucose was 180. He ended up in ICU for three days. The drug wasn’t the villain-it was the combo. Stress, fasting, alcohol, and no insulin buffer. That’s the perfect storm. Know your triggers. Protect yourself.
Kitty Price
December 25, 2025 AT 12:42Just got my ketone strips in the mail 😊 I’m keeping them next to my glucose meter. I’m on canagliflozin 100mg and had a cold last month-felt awful but my sugar was ‘normal.’ Now I know better. Thanks for the heads up! 🙏
Kim Hines
December 27, 2025 AT 01:08I’m on empagliflozin. I’ve never had any issues. I eat normally, I’m not fasting, I’m not sick. I think people are overreacting. If you’re doing everything right, you’re fine. Don’t panic because of scary stories.
Joanna Ebizie
December 28, 2025 AT 17:02Wow. So you’re telling me I’m supposed to stop my weight loss drug every time I get a cold? That’s ridiculous. You’re scaring people for no reason. If you’re not diabetic enough to get DKA, you’re fine. Stop being paranoid and just take your pill.