Thiazide Diuretic Gout Risk Calculator
Gout Risk Assessment
This calculator estimates your risk of developing gout while taking thiazide diuretics based on your medical history and lifestyle factors.
Risk Assessment Results
Key Information
Thiazide diuretics can raise uric acid levels by 6-21% within days. Uric acid levels above 6.8 mg/dL increase gout risk.
If you're taking a thiazide diuretic like hydrochlorothiazide for high blood pressure, you might not realize it could be raising your risk of gout. It’s not a common side effect for everyone, but for some people, especially those with a history of high uric acid or past gout attacks, this medication can trigger painful flare-ups. The connection isn’t guesswork-it’s backed by decades of research and clinical data. And if you’re one of the 50 million Americans prescribed a thiazide each year, understanding this link could help you avoid unnecessary pain and extra medications.
How Thiazide Diuretics Raise Uric Acid Levels
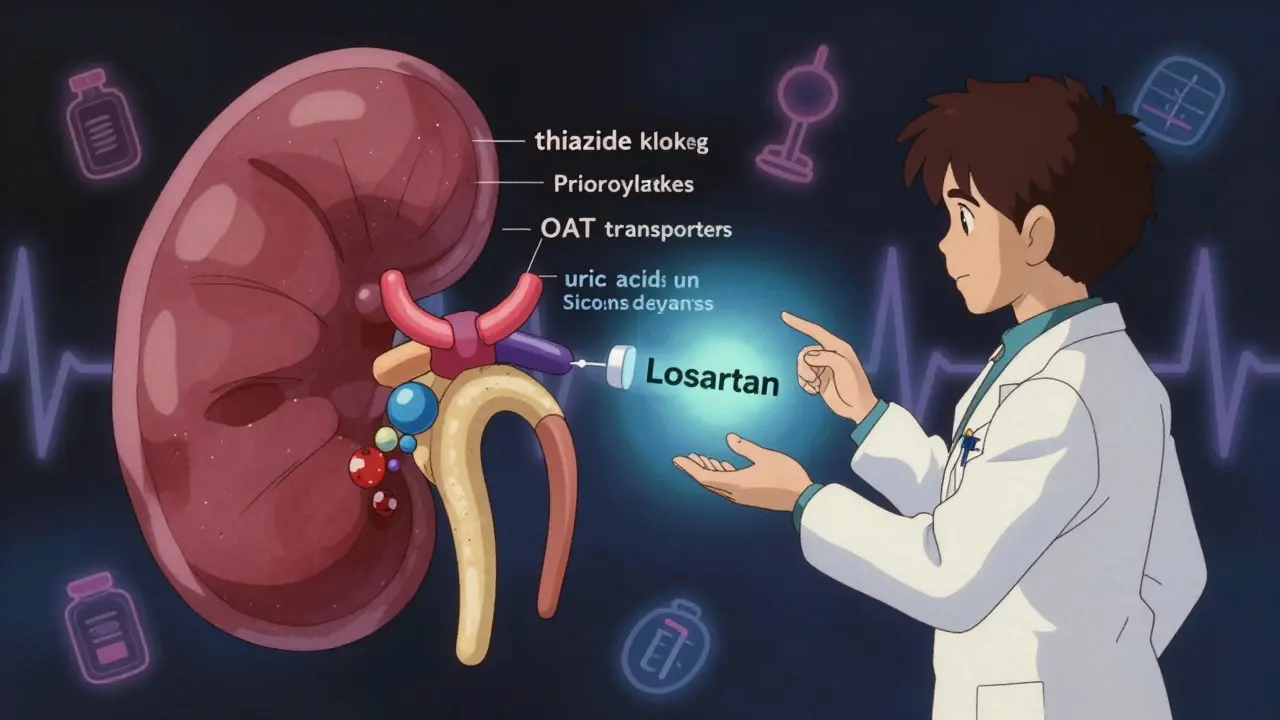
Thiazide diuretics, including hydrochlorothiazide and chlorthalidone, work by making your kidneys flush out more sodium and water. That lowers blood pressure. But here’s the catch: they also mess with how your kidneys handle uric acid. Uric acid is a waste product from breaking down purines in food. Normally, your kidneys filter it out and send it through urine. But thiazides interfere with that process.
Research shows these drugs compete with uric acid for transporters in the kidney, especially OAT1 and OAT4. When thiazides latch onto these transporters, uric acid gets trapped in the bloodstream instead of being excreted. The result? Your serum uric acid levels can rise 6% to 21% within just a few days of starting the drug. This isn’t a slow build-it happens fast. And if your levels cross 6.8 mg/dL, the point where uric acid starts crystallizing, you’re at risk for gout.
Who’s Most at Risk?
Not everyone who takes a thiazide gets gout. But certain people are far more likely to. If you already have high uric acid (above 7.0 mg/dL for men, 6.0 mg/dL for women), a past gout attack, or kidney problems, your risk jumps. Genetics matter too. Some people naturally reabsorb more uric acid in their kidneys, and thiazides make that worse.
Studies show the longer you take thiazides, the higher your risk. After 180 days of use, the chance of needing gout medication rises by 41% compared to the first month. That’s not a small increase. And it’s not just about the drug-it’s about timing. Many people start taking allopurinol or colchicine months after beginning thiazides, not because their gout got worse, but because the medication itself triggered it. This is called a prescribing cascade: one drug causes a problem that leads to another drug, which might not be needed if the original trigger was avoided.
Thiazides vs. Other Diuretics
Not all diuretics are the same when it comes to gout. Loop diuretics like furosemide carry an even higher risk than thiazides. But among thiazides themselves, there’s a myth that chlorthalidone is worse than hydrochlorothiazide. Recent studies say that’s not true. At similar doses, both drugs raise uric acid about the same. So switching from one to the other won’t solve the problem if you’re already at risk.
On the flip side, potassium-sparing diuretics like spironolactone don’t raise uric acid at all. In fact, they might even help lower it slightly. That makes them a smart alternative for people with both high blood pressure and a history of gout.
What Does Gout Look Like When It’s Triggered by Thiazides?
There’s nothing special about gout caused by thiazides. It looks exactly like any other gout attack: sudden, intense pain in one joint-usually the big toe. The joint swells, turns red, and feels hot to the touch. It often hits at night and can be so painful you can’t even tolerate a bedsheet touching it. Blood tests will show uric acid above 6.8 mg/dL in about 90% of cases. But here’s the twist: some people have high uric acid without symptoms, and others get attacks even with normal levels. That’s why doctors don’t rely on blood tests alone to diagnose gout-they look at the symptoms and sometimes use imaging or joint fluid tests.
What Should You Do If You’re on Thiazides?
If you’re taking a thiazide and have never had gout, you don’t need to panic. Only 1-2% of people on these drugs develop gout. But if you have risk factors-like high uric acid, obesity, heavy alcohol use, or a family history of gout-you should talk to your doctor. The American College of Cardiology recommends checking your uric acid level before starting thiazides if you have any of these risk factors. That simple step can prevent a lot of trouble down the road.
If you’ve already had a gout attack and your doctor wants to keep you on a thiazide, they should also prescribe a urate-lowering drug like allopurinol. The European League Against Rheumatism recommends keeping uric acid below 6.0 mg/dL to prevent crystals from forming. Lifestyle changes matter too: cut back on beer, red meat, shellfish, and sugary drinks. Losing even 5-10% of your body weight can cut your gout risk in half.

Alternatives to Thiazides That Don’t Raise Uric Acid
You don’t have to stay on thiazides if they’re causing problems. There are other blood pressure medications that won’t raise uric acid-and some might even help lower it.
- Losartan: This is an ARB, a type of blood pressure drug that blocks angiotensin II. Unlike other ARBs, losartan also blocks the URAT1 transporter in the kidney, which helps your body get rid of more uric acid. It’s a double win: lowers blood pressure and uric acid.
- Calcium channel blockers: Drugs like amlodipine and diltiazem don’t affect uric acid at all. They’re just as effective as thiazides for lowering blood pressure.
- Spironolactone: This potassium-sparing diuretic doesn’t interfere with uric acid excretion. It’s especially useful if you have heart failure or resistant hypertension.
Yes, some of these alternatives cost more. Generic hydrochlorothiazide runs about $4 for 90 pills. Losartan and amlodipine are also cheap generics now, but prices vary. Still, if you’re spending hundreds a year on gout meds because of thiazide-induced flare-ups, switching might save you money in the long run.
The Bigger Picture: Blood Pressure vs. Gout
Here’s the tricky part: high blood pressure and gout are linked in both directions. People with high blood pressure are nearly twice as likely to get gout. And people with high uric acid are more likely to develop high blood pressure. That makes it hard to tell what’s causing what in some cases. But the evidence is clear: thiazides add fuel to the fire. They don’t just coincide with gout-they actively raise the risk.
That’s why major guidelines now say: don’t use thiazides alone if you have gout or uric acid over 8.0 mg/dL. If you must use them, pair them with a urate-lowering drug. The cardiovascular benefits of controlling blood pressure are real-heart attacks and strokes are serious. But so is chronic joint damage from repeated gout attacks. The goal isn’t to avoid thiazides entirely. It’s to use them wisely.
What’s Next for Thiazides?
Researchers are working on new diuretics that lower blood pressure without messing with uric acid. A new drug in Phase II trials (NCT04892105) targets only the sodium-chloride cotransporter in the kidney, avoiding the OAT transporters that move uric acid. Results aren’t expected until late 2025, but if it works, it could change how we treat hypertension in people with gout.
In the meantime, the best approach is awareness. If you’re on a thiazide and have any risk factors for gout, ask your doctor about your uric acid level. If you’ve had a gout attack since starting the drug, don’t assume it’s just bad luck. Ask if the medication could be the cause-and whether a safer alternative exists.
Can thiazide diuretics cause gout even if I’ve never had it before?
Yes. While only 1-2% of people on thiazides develop gout, it can happen even without a prior history. The risk increases with longer use, higher doses, and other factors like obesity, alcohol use, or kidney issues. Symptoms usually appear after several months of use, not immediately.
Should I stop taking hydrochlorothiazide if I develop gout?
Not necessarily. Stopping the drug may help, but it’s not always the best choice. If you need it for blood pressure control, your doctor may recommend keeping it while adding a urate-lowering drug like allopurinol. Stopping abruptly can cause your blood pressure to spike, which is dangerous. Always talk to your doctor before making changes.
Is chlorthalidone worse than hydrochlorothiazide for gout?
No. Earlier beliefs suggested chlorthalidone raised uric acid more, but recent studies show both drugs have nearly identical effects on uric acid levels at standard doses. Switching between them won’t reduce your gout risk.
How long does it take for uric acid levels to return to normal after stopping thiazides?
Typically, uric acid levels begin dropping within weeks and return to baseline within 2-3 months after stopping the drug. However, if crystals have already formed in your joints, gout attacks may continue for months until the crystals dissolve, even after levels normalize.
Are there any blood pressure meds that help lower uric acid?
Yes. Losartan, an ARB, helps your kidneys excrete more uric acid by blocking the URAT1 transporter. Calcium channel blockers and spironolactone have no effect on uric acid and are safe alternatives. Losartan is often preferred for patients with both hypertension and gout.







Candice Hartley
January 26, 2026 AT 23:46My dad just got diagnosed with gout after 2 years on HCTZ. I wish we’d known this sooner.
April Williams
January 28, 2026 AT 03:10Of course the medical establishment ignores this until people are in agony. They’d rather prescribe another pill than admit their first one is broken. Wake up, people. This isn’t medicine, it’s profit-driven negligence.
Harry Henderson
January 28, 2026 AT 23:06STOP TAKING THIAZIDES IF YOU’RE AT RISK. PERIOD. LOSARTAN IS FREE, EFFECTIVE, AND ACTUALLY HELPS YOUR URIC ACID. YOUR DOCTOR ISN’T YOUR FRIEND IF THEY KEEP YOU ON THIS DRUG WITHOUT A PLAN. DO THE RESEARCH. SAVE YOUR JOINTS.
suhail ahmed
January 30, 2026 AT 13:51Bro, this is why I tell my patients in Delhi: if you’re from a family where gout runs deep, don’t let your doctor just hand you HCTZ like candy. I’ve seen men in their 40s lose the ability to walk because no one checked uric acid before prescribing. Losartan isn’t just an alternative-it’s a gift. And yes, it’s cheap as hell now. Your kidneys will thank you. Your big toe will too.
Paul Taylor
February 1, 2026 AT 02:27I’ve been on chlorthalidone for 7 years and my uric acid went from 5.8 to 8.2 in 18 months. No gout attacks yet but I’ve been living with this constant low-grade joint stiffness and I thought it was just aging. Turns out it was the drug. I switched to amlodipine last month. My levels are down to 6.1. The difference isn’t dramatic but I can finally put on socks without wincing. I wish someone had told me this before I lost two years of my life thinking it was normal.
Kegan Powell
February 2, 2026 AT 22:53It’s wild how we treat blood pressure like it’s the only thing that matters when your body is screaming in pain. Gout isn’t just a bad toe-it’s inflammation that eats at your bones over time. And we’re just handing out thiazides like they’re candy because the numbers look good on paper. But if you’re not feeling well, what’s the point? Losartan does the job and quietly helps your body clean up the mess. Why aren’t we starting there? Maybe because it’s not the default. But maybe it should be.
John O'Brien
February 3, 2026 AT 15:58my doc told me to stop hctz and switch to lisinopril and i thought he was crazy. turns out lisinopril raises uric acid too. i ended up on losartan and my toe hasn’t hurt since. also lost 12 lbs and cut out beer. no joke. life changed.
Andrew Clausen
February 4, 2026 AT 08:53Let’s be clear: the 1–2% statistic is misleading. It’s not that thiazides cause gout in 1–2% of people-it’s that 1–2% of people develop *symptomatic* gout. The real number of people with elevated uric acid from these drugs is closer to 30–40%. The medical community doesn’t track asymptomatic hyperuricemia because it doesn’t pay. But if you’re taking thiazides and have any risk factors, you’re playing Russian roulette with your joints. Don’t wait for the bullet.