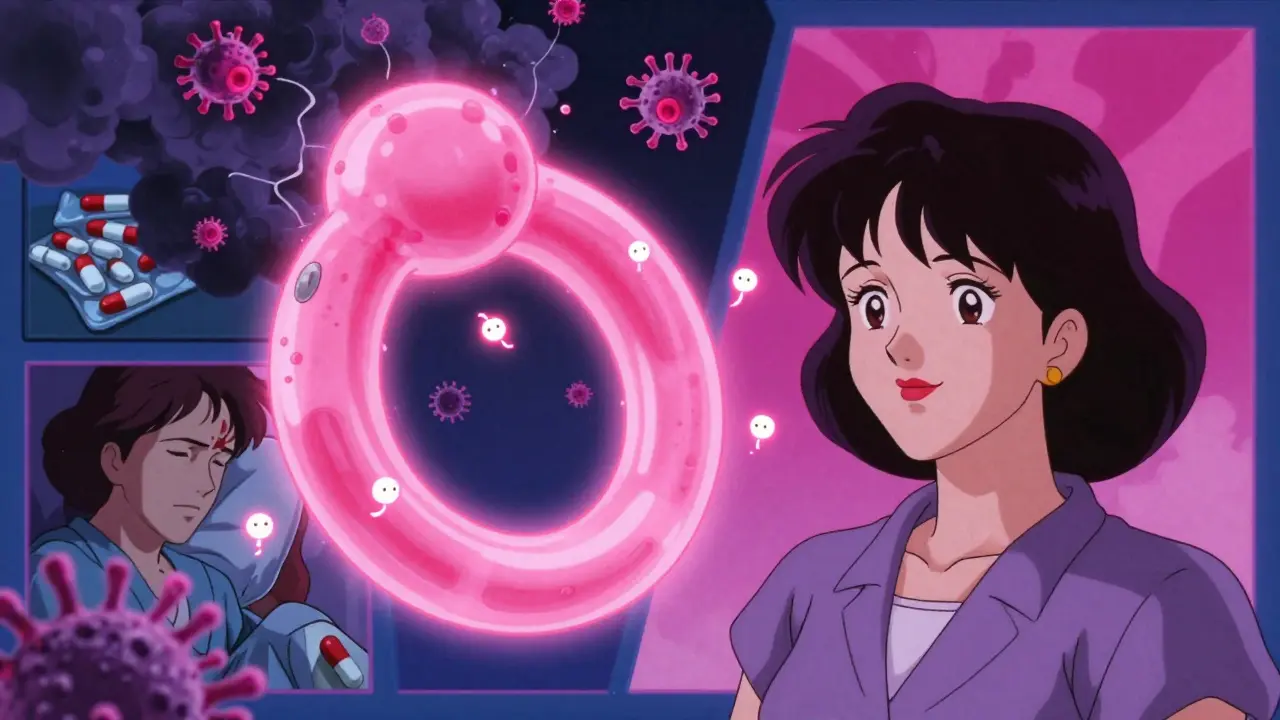
Every year, about 8 to 10 million people in the U.S. visit their doctor because of a urinary tract infection. That’s more than the number of people who get the flu. Most of them are women. And while it’s common, it’s not something you should ignore. A UTI isn’t just a nuisance-it can turn dangerous fast if left untreated.
What Causes a Urinary Tract Infection?
A urinary tract infection happens when bacteria sneak into your urinary system. That includes your bladder, urethra, ureters, or even your kidneys. The most common culprit? Escherichia coli-a type of bacteria that normally lives in your gut. It gets pulled into the urethra, usually from the anus, and climbs up.Women are way more likely to get UTIs than men. Why? Because women have a much shorter urethra-only about 4 centimeters long. That’s like a straight shot from outside to bladder. Men have a urethra that’s about five times longer, which gives bacteria a harder time reaching the bladder.
Other things that raise your risk:
- Sexual activity-especially if you’re new to a partner or having sex more often
- Using spermicides or diaphragms-these can kill off good bacteria and let bad ones take over
- Menopause-lower estrogen means thinner tissue around the urethra, making it easier for bacteria to stick
- Not emptying your bladder fully-holding it in too long lets bacteria multiply
- Having a catheter or other urinary device
It’s not just about hygiene. You can be perfectly clean and still get a UTI. It’s anatomy, not dirt.
How Do You Know You Have a UTI?
The signs are hard to miss if you’ve had one before. But if it’s your first time, you might think it’s just a bad period cramp or a stomach bug.For a lower UTI (bladder or urethra), you’ll likely feel:
- Burning when you pee-this hits 92% of patients
- Needing to go all the time, even if you just went
- A sudden, strong urge to pee
- Pressure or pain in your lower belly
- Cloudy, strong-smelling, or bloody urine
If the infection moves up to your kidneys (pyelonephritis), things get serious fast:
- Flank pain-sharp pain on one side of your lower back
- Fever over 101°F
- Nausea or vomiting
- Chills
These symptoms mean you need to see a doctor right away. Kidney infections can lead to sepsis, especially in older adults or people with weakened immune systems.
What Antibiotics Actually Work?
Not all antibiotics are created equal for UTIs. The right one depends on where you live, your medical history, and whether the infection is simple or complicated.For a first-time, uncomplicated bladder infection, doctors usually start with one of these:
- Nitrofurantoin-100 mg twice a day for 5 days. Works great for the bladder. But don’t use it if you think your kidneys are involved-it doesn’t reach them well.
- Trimethoprim-sulfamethoxazole (Bactrim)-160/800 mg twice a day for 3 days. Used to be the gold standard, but resistance is up to 30% in many U.S. areas now.
- Fosfomycin-a single 3-gram dose. Convenient, and less likely to cause yeast infections.
For more serious cases-like kidney infections or if you’ve had multiple UTIs-you might need:
- Ciprofloxacin (Cipro)-500 mg twice daily for 7 to 14 days. Powerful, but linked to tendon damage and nerve issues. Doctors now avoid it unless absolutely necessary.
- Ceftriaxone-an IV antibiotic given in the hospital for severe cases.
Here’s the catch: Antibiotic resistance is rising. In some parts of the country, more than 30% of E. coli strains don’t respond to Bactrim anymore. That’s why your doctor might ask for a urine culture before prescribing-especially if you’ve had UTIs before.

Can You Prevent UTIs Without Antibiotics?
Yes. And many people who get repeat UTIs are tired of popping pills every few months. Prevention works better than treatment for most.Here’s what actually helps, backed by science:
- Drink water. Aim for at least 1.5 liters a day. A 2022 study found women who drank more water cut their UTI risk by almost half.
- Pee after sex. It flushes out bacteria before they can climb up. Reduces risk by about 50%.
- Avoid spermicides. Nonoxynol-9 kills good bacteria and makes UTIs more likely. Switch to condoms without it.
- Wipe front to back. Sounds basic, but it’s the #1 thing you can do at home to stop bacteria from traveling.
Some supplements show real promise:
- D-mannose-2 grams a day. A 2021 study found it worked better than antibiotics at preventing recurrences. It sticks to E. coli and lets your body flush it out.
- Cranberry-but only if it’s high in PACs (proanthocyanidins). Most store-bought juices and gummies have almost none. Look for supplements with at least 36 mg PACs daily.
- Vaginal estrogen-for postmenopausal women. A thin cream or ring applied twice a week can slash UTI rates by 70%.
One study followed women who used D-mannose for a year. They cut their antibiotic use in half. That’s huge.
What About Home Tests and Self-Treatment?
You can buy UTI test strips at any pharmacy. They check for nitrites and white blood cells in your urine. They’re fast and easy-but they’re not perfect. About 1 in 4 results are false negatives. That means you could have an infection and the test says you’re fine.Some people try to treat mild symptoms on their own. One BMJ study found that 25-43% of uncomplicated UTIs clear up without antibiotics. But here’s the risk: If you wait too long, it can spread to your kidneys. And if you’re over 65, pregnant, diabetic, or have a catheter-don’t wait. Go to the doctor.
For quick relief, some use phenazopyridine (Pyridium). It numbs the bladder lining and stops the burning within 20 minutes. But it turns your pee bright orange. And it doesn’t treat the infection-it just hides the pain.
What’s New in UTI Treatment?
The last new antibiotic approved for UTIs in the U.S. was over 20 years ago. That’s changing.In 2024, the FDA approved gepotidacin, a brand-new oral antibiotic that works against drug-resistant E. coli. In trials, it cured 92% of cases. It’s not widely available yet, but it’s a big step.
There’s also a new class of drugs called FimH inhibitors. One, EB8018, blocks bacteria from sticking to the bladder wall. In trials, it cut recurrence by 75% compared to placebo.
And researchers are testing vaginal probiotics-specifically Lactobacillus crispatus. In a 2024 study, women who used suppositories with this strain had 55% fewer UTIs. It’s like restoring the right kind of bacteria to keep the bad ones out.
What to Do If You Keep Getting UTIs
If you’ve had three or more UTIs in a year, you’re not alone. About 1 in 3 women will have a repeat infection. But you don’t have to live like this.Doctors have two proven strategies for recurrent UTIs:
- Post-sex prophylaxis-take a low-dose antibiotic (like nitrofurantoin or trimethoprim) within 2 hours after sex. Cuts recurrence by 95%.
- Low-dose daily antibiotics-take a tiny amount every night for 6 months. Reduces episodes from nearly 7 a year to less than 1.
Many people avoid this because they’re scared of resistance. But for recurrent cases, the benefit outweighs the risk. And you can switch to D-mannose or cranberry after 6 months to wean off antibiotics.
Also, talk to your doctor about your menopause status. Estrogen loss is a hidden cause of recurring UTIs in women over 50. A simple vaginal estrogen treatment can be life-changing.
When to See a Doctor
Don’t wait if:- You have fever, chills, or back pain
- You’re pregnant
- You’re over 65
- You have diabetes or a weakened immune system
- Your symptoms don’t improve in 48 hours after starting antibiotics
- You keep getting UTIs-more than two a year
And if you’ve been treated for a UTI multiple times but still feel symptoms? You might have something else-like interstitial cystitis or a bladder stone. About 4 in 10 people are misdiagnosed at first. A proper urine culture and maybe a referral to a urologist can make all the difference.
Can UTIs go away on their own without antibiotics?
Yes, in some cases. About 25-43% of uncomplicated bladder infections clear up on their own, especially if you drink plenty of water and pee often. But this isn’t safe for everyone. If you’re elderly, pregnant, diabetic, or have a catheter, waiting can lead to kidney infection or sepsis. Don’t gamble with your health-see a doctor if symptoms last more than 24 hours.
Why do I keep getting UTIs after sex?
Sex can push bacteria from the anus or skin into the urethra. Women are especially vulnerable because of their short urethra. To reduce risk, pee within 30 minutes after sex. Avoid spermicides and diaphragms. If it keeps happening, ask your doctor about taking a single low-dose antibiotic right after intercourse. This cuts recurrence by 95%.
Is cranberry juice good for UTIs?
Most cranberry juice isn’t strong enough. The active ingredient, PACs (proanthocyanidins), needs to be in high doses-36 mg per day-to work. A glass of juice has maybe 1-2 mg. Look for supplements labeled with PAC content. Avoid sweetened juices-they’re just sugar water with a hint of cranberry.
Can men get UTIs?
Yes, but it’s less common. When men get UTIs, it’s often linked to an underlying issue-like an enlarged prostate, kidney stones, or a catheter. UTIs in men are more likely to be complicated and need longer treatment. Never ignore UTI symptoms in men-see a doctor right away.
Do UTI test strips really work?
They’re helpful for spotting possible infections, but they’re not foolproof. About 20-30% of the time, they give false negatives-you can have a UTI and the strip says you don’t. They also can’t tell you which bacteria is causing it. If you have symptoms but the test is negative, still see a doctor. A urine culture is the gold standard.
What’s the best way to prevent a UTI after menopause?
Low-dose vaginal estrogen is the most effective option. As estrogen drops, the tissue around the urethra thins and dries out, making it easier for bacteria to stick. Applying a small amount of estrogen cream or using a ring twice a week can reduce UTIs by 70%. It’s safe, local, and doesn’t affect your whole body. Talk to your gynecologist or primary care provider about it.
Final Thoughts
UTIs are common, but they’re not normal. Just because you’ve had one before doesn’t mean you have to keep having them. The key is knowing the triggers, using the right prevention tools, and not letting fear of antibiotics stop you from getting help when you need it.Drink water. Pee after sex. Skip the spermicides. Try D-mannose or vaginal estrogen if you’re postmenopausal. And if you’re still getting infections-don’t just tough it out. There are better ways now. New treatments are coming. Prevention works. You don’t have to live with this.







Ryan van Leent
December 19, 2025 AT 00:43Meenakshi Jaiswal
December 19, 2025 AT 01:02Dikshita Mehta
December 19, 2025 AT 04:16Marsha Jentzsch
December 20, 2025 AT 01:05Kathryn Featherstone
December 20, 2025 AT 06:22Dominic Suyo
December 21, 2025 AT 08:49Kevin Motta Top
December 22, 2025 AT 13:08Dev Sawner
December 24, 2025 AT 09:52pascal pantel
December 26, 2025 AT 06:17Anna Sedervay
December 26, 2025 AT 23:33James Stearns
December 28, 2025 AT 01:47Alisa Silvia Bila
December 28, 2025 AT 09:04Moses Odumbe
December 29, 2025 AT 12:13Carolyn Benson
December 30, 2025 AT 14:54Henry Marcus
December 31, 2025 AT 06:58