Every year, thousands of young children end up in emergency rooms because they got into medicine they weren’t supposed to. It’s not because parents are careless-it’s because the risks are hidden in plain sight. A bottle left on the nightstand. A teaspoon used to measure liquid medicine. A child-resistant cap that wasn’t clicked shut. These aren’t rare mistakes. They’re common, preventable, and often deadly.
Why This Happens More Than You Think
Children under five are natural explorers. They grab, taste, and test everything. That’s developmentally normal. But it makes them dangerously vulnerable to accidental overdoses. The CDC reports that in 2010, emergency departments saw over 76,000 cases of unsupervised medication exposure in kids under five. That’s more than 200 cases a day. And while numbers have dropped since then, the threat hasn’t gone away. The most common culprits? Liquid acetaminophen and diphenhydramine. Together, they account for nearly half of all pediatric medication overdoses. Why? Because they’re everywhere-cough syrups, sleep aids, allergy meds. And they come in different concentrations. One bottle says “infant drops,” another says “children’s syrup.” They look almost identical. But the strength? Totally different. Mix them up, and you’re giving your child five times the dose they should get.What Actually Works to Prevent It
The CDC’s PROTECT Initiative isn’t just a slogan. It’s a proven, three-part system that’s cut pediatric medication overdoses by 25% since 2010. And it’s built on simple, doable steps.- Store meds out of sight and reach. Not on the counter. Not on the nightstand. Not in a purse on the couch. Locked cabinet. At least four feet off the ground. Even toddlers can climb. A 2023 Reddit post from a parent tells the story: their 2-year-old got into blood pressure pills because they were left on the bedside table after a doctor’s visit. One mistake. One terrifying hour in the ER.
- Use only the dosing tool that comes with the medicine. Kitchen spoons are not accurate. A tablespoon isn’t the same as a milliliter. A 2022 analysis of 1,200 cases found that 78% of dosing errors came from using spoons, cups, or syringes not meant for medicine. The bottle says 5 mL? Use the syringe that came with it. Not the one from last time. Not the one you think is close enough.
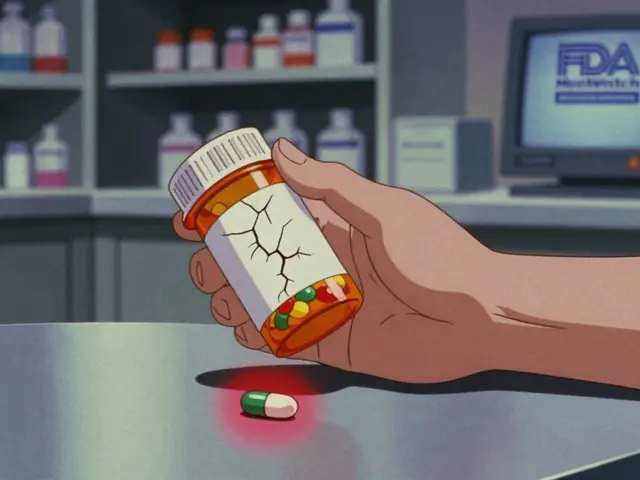
- Keep everything in original bottles. Don’t dump pills into a pill organizer unless you’re 100% sure you won’t mix them up. Don’t pour liquid meds into unlabeled containers. Original labels have the concentration, expiration date, and dosing instructions. Lose that, and you’re guessing.
How to Measure Medicine Right
Since 2019, federal rules have required all pediatric liquid medications to list doses in milliliters (mL) only. No more teaspoons, tablespoons, or drams. That’s a big win. But not every manufacturer followed through perfectly. Some still include old measurements in small print. Always read the label twice. If it says “5 mL,” don’t assume it’s one tablespoon. It’s not. One tablespoon is 15 mL. That’s three times too much. If you’re given a syringe or cup, make sure it matches the dose. If the bottle says 1.25 mL, and your syringe only has marks at 1 mL and 2 mL, ask for a better one. Pharmacies have them. Don’t wing it.
What to Do If Your Child Gets Into Medicine
If you think your child swallowed something they shouldn’t, don’t wait. Don’t call your pediatrician first. Don’t Google symptoms. Call poison control immediately: 1-800-222-1222. It’s free, it’s 24/7, and they know exactly what to do. If it’s an opioid-like codeine, oxycodone, or fentanyl-and your child is unresponsive, not breathing, or turning blue, give naloxone if you have it. Yes, naloxone is approved for kids. Yes, it works. But most families don’t have it. The American Academy of Pediatrics now recommends that any child prescribed opioids also get a prescription for naloxone. If your child’s doctor didn’t mention it, ask. Don’t assume it’s only for adults. Don’t try to make your child vomit. Don’t give them milk or charcoal unless poison control tells you to. Time matters. The faster you act, the better the outcome.Why Many Parents Still Get It Wrong
Even with all the education, only 32% of households store medications in locked cabinets. Only 58% use child-resistant caps correctly. Why? Because it’s easy to forget. You’re tired. You’re in a rush. You think, “I’ll just put it here for now.” But “for now” becomes “all day.” And “all day” becomes an emergency. A 2022 survey of pediatricians found that only 63% consistently talk to parents about safe storage during checkups. That’s not enough. Prevention isn’t just the parent’s job-it’s the system’s job too. And while smart packaging and automated dispensers exist (like Hero Health or AdhereIT), they cost hundreds of dollars. Most families can’t afford them. That’s why the simple, free solutions-locked cabinets, proper dosing tools, calling poison control-still matter most.
What’s Changing Now
The FDA is set to require flow restrictors on all liquid opioid medications by 2025. That’s a small plastic valve inside the bottle that slows the flow so a child can’t pour out a full dose. It’s already used in some adult medications. It’s coming to kids’ meds next. The CDC’s Up and Away campaign is expanding into 12 new languages by 2026. That’s huge. Language barriers are a major reason why non-English-speaking families don’t know how to store meds safely. And in 2024, the AAP released its first-ever clinical guideline for prescribing opioids to children. It says: if you give an opioid, you must also give naloxone and teach parents how to use it. That’s a game-changer.What You Can Do Today
You don’t need a fancy device. You don’t need a PhD in pharmacology. You just need to make three changes:- Find every medicine in your house-prescription, OTC, vitamins, even old ones from last winter. Put them in one place.
- Lock them up. A high cabinet with a latch is enough. Even a small lockbox from the hardware store works.
- Keep the dosing tool with the bottle. Never use a kitchen spoon. Never guess.
Final Thought
Accidental overdoses aren’t about bad parenting. They’re about systems that don’t make safety easy. But you don’t have to wait for the system to fix itself. You can act today. Lock the cabinet. Use the right syringe. Know the number. These aren’t just tips-they’re lifesavers.What should I do if my child swallows medicine they weren’t supposed to?
Call poison control immediately at 1-800-222-1222. Do not wait for symptoms. Do not try to make your child vomit. Have the medicine container ready when you call-this helps them give you the right advice. If your child is unresponsive, not breathing, or turning blue, and you have naloxone, use it right away and call 911.
Are child-resistant caps enough to keep kids safe?
No. Child-resistant caps are designed to slow down kids, not stop them. Studies show 10% of children can open them by age 3.5. That’s why storing medicine in a locked cabinet, at least four feet off the ground, is critical. Caps are a backup, not a solution.
Can I use a kitchen spoon to measure liquid medicine?
Never. Kitchen spoons vary in size. A tablespoon can hold anywhere from 13 to 20 milliliters. Medicine doses are measured in milliliters (mL), and even a small difference can be dangerous. Always use the syringe, dropper, or cup that came with the medicine.
Is naloxone safe for young children?
Yes. Naloxone is FDA-approved for children and can reverse opioid overdoses at any age. The American Academy of Pediatrics now recommends that any child prescribed an opioid also be given naloxone. It’s safe, fast-acting, and can save a life. If your child’s doctor doesn’t offer it, ask for it.
What’s the difference between infant and children’s acetaminophen?
Infant drops are more concentrated-80 mg per 0.8 mL. Children’s syrup is less concentrated-160 mg per 5 mL. If you give infant drops using the syrup dosing instructions, you’ll give your child five times the intended dose. Always check the label. Never assume they’re the same.
How do I safely dispose of old or unused medications?
Use a drug take-back program if available. Many pharmacies and police stations offer them. If not, mix pills with used coffee grounds or cat litter, seal them in a container, and throw them in the trash. Don’t flush them unless the label says to. For liquids, pour them into a sealable bag with kitty litter or sawdust before disposal.
Why do some medications still have teaspoon measurements on the label?
Federal law now requires all pediatric liquid medications to list doses only in milliliters (mL). But some older products or generics may still have teaspoons in small print. Always follow the mL measurement. If you’re unsure, ask your pharmacist to clarify.
Are smart medication dispensers worth the cost?
They can help, but they’re expensive-often over $300-and not covered by insurance. Most families can’t afford them. The most effective prevention is free: locked storage, proper dosing tools, and knowing the poison control number. Don’t wait for tech to solve this. Start with what you have.






Hannah Gliane
February 3, 2026 AT 06:26OMG I literally just found my 2-year-old with a bottle of Children’s Benadryl in her mouth yesterday 😱 I thought I locked it up but nope - it was on the nightstand ‘for easy access’ because I was ‘just going to take it after her bath’… 🤦♀️ I called poison control and they were SO calm. I’m now the queen of the locked cabinet. Also, why do pharmacies still give you a spoon???
Murarikar Satishwar
February 3, 2026 AT 22:26Excellent and comprehensive guide. As a pediatric nurse in India, I’ve seen too many cases where parents use kitchen spoons because they don’t have the dosing syringe, or because they believe ‘a little more won’t hurt.’ The cultural normalization of improvisation with medications is dangerous. I always carry spare syringes in my clinic bag and give them out free. Simple tools save lives. Also, the point about infant vs. children’s acetaminophen is critical - I’ve seen families confuse the two even after being shown twice. Labels must be read aloud, together, every time.
Marc Durocher
February 5, 2026 AT 07:13Y’all are acting like this is some new revelation. I’ve been locking my meds since my kid turned 6 months. The real problem? The fact that we’re still having this conversation in 2025. Like, we’ve had child-resistant caps since the 70s, yet somehow we still need a Reddit post to tell us not to leave pills on the nightstand? 🤡 Also - why does poison control even exist as a separate entity? Shouldn’t this be common sense? Anyway, glad the FDA’s finally forcing flow restrictors. Took long enough.
Akhona Myeki
February 6, 2026 AT 18:36Let me be clear: this is not a parenting issue. This is a systemic failure of American healthcare. In South Africa, we don’t have the luxury of over-the-counter cough syrups in every corner store. Our medications are regulated, stored centrally, and dispensed by trained pharmacists. We don’t need Reddit posts to tell us not to use teaspoons - because we don’t have teaspoons for medicine. The fact that this is even a debate in the U.S. is a disgrace. Locking cabinets? That’s step one. Step two: stop selling dangerous products to the public like candy.
Gary Mitts
February 7, 2026 AT 21:33clarissa sulio
February 9, 2026 AT 19:48I read this whole thing and I’m still mad. Why is this even a thing? Why are we letting companies sell two different concentrations of the same drug that look identical? Why are pharmacies still giving out measuring cups that aren’t calibrated? This isn’t a parenting problem - it’s a corporate negligence problem. I’m not blaming anyone. I’m just saying - if this was a car seat or a crib, we’d have lawsuits and recalls. But pills? Nah. Just lock them up. Like we’re the villains here.
Bridget Molokomme
February 11, 2026 AT 10:52Okay but real talk - I’ve been using the same syringe for three kids and three different meds. I just rinse it out. Is that bad? I mean… it’s not like I’m using a dirty spoon. But now I’m paranoid. Should I be buying a new one every time? Also - why does the pharmacy charge $4 for a new syringe? It’s plastic. It’s 2 inches long. I can buy 100 of these on Amazon for $3. Someone’s making a killing off parental guilt.
Vatsal Srivastava
February 12, 2026 AT 18:25Interesting how everyone treats this like a universal truth. But what if the real issue is that we’re over-medicalizing childhood? A little acetaminophen here, a little diphenhydramine there - maybe we don’t need to treat every sniffle. Maybe the problem isn’t storage - it’s prescribing. Why are we giving kids OTC meds like they’re candy? Maybe the solution isn’t locking cabinets… it’s reducing reliance on drugs altogether.
Brittany Marioni
February 13, 2026 AT 18:15I just want to say, thank you for writing this. I’m a single mom of three, working two jobs, and I didn’t even know about the infant vs. children’s concentration difference. I’ve been using the same syringe for years. I’ve used the kitchen spoon. I’ve left meds on the counter. I thought I was being practical. Now I feel awful. But I’m fixing it. I bought a lockbox today. I’m throwing out all the old bottles. I’m calling poison control tomorrow just to say hi. You’re right - this isn’t about being perfect. It’s about being aware. And you made me aware. Thank you.