Antihistamine Interaction Checker
Check Your Medication Combination
This tool helps identify dangerous combinations between antihistamines and other sedating medications. Enter your medications below to see if there are risks.
Results
How to Use This Tool
- First-generation antihistamines (Benadryl, Vistaril, Phenergan) are the most dangerous
- Always check all medications, including over-the-counter drugs and alcohol
- Older adults and people with liver/kidney issues are at higher risk
- Second-generation antihistamines (Claritin, Zyrtec, Allegra) are safer alternatives
Combining antihistamines with other sedating drugs can be dangerous - and many people don’t realize it until it’s too late. If you’re taking Benadryl for allergies, sleeping pills for insomnia, or even just a muscle relaxer for back pain, you might be putting yourself at risk without knowing it. The problem isn’t just drowsiness. It’s slowed breathing, confusion, falls, and in worst-case scenarios, hospitalization or death. This isn’t theoretical. Every year, over 300,000 emergency room visits in the U.S. are linked to dangerous drug combinations involving antihistamines and other CNS depressants.
Why First-Generation Antihistamines Are the Main Problem
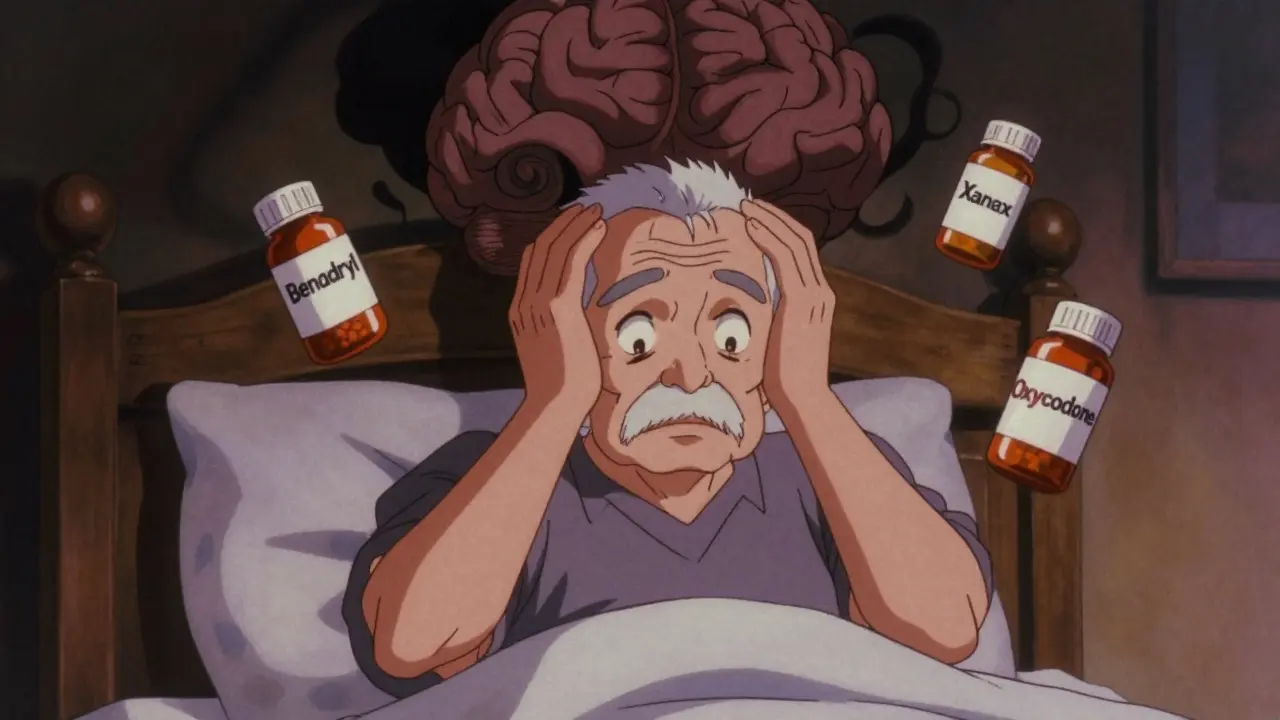
Not all antihistamines are the same. There are two main types: first-generation and second-generation. The first-generation ones - like diphenhydramine (Benadryl), hydroxyzine (Vistaril), and promethazine (Phenergan) - were developed in the 1940s. They work well for allergies, motion sickness, and even as sleep aids. But they cross the blood-brain barrier easily. That’s why they make you sleepy. And that’s also why they’re risky when mixed with other sedating drugs.These medications don’t just block histamine. They also act as anticholinergics, meaning they interfere with acetylcholine, a brain chemical critical for memory, focus, and muscle control. On the Anticholinergic Cognitive Burden (ACB) scale, diphenhydramine scores a 3 - the highest level. That means even one dose can impair thinking in older adults. Combine that with a benzodiazepine like Xanax or a painkiller like oxycodone, and the effect isn’t just additive - it’s multiplied.
Studies show that when diphenhydramine is taken with lorazepam (Ativan), sedation increases by 37% in objective tests. Subjective drowsiness jumps by 42%. That’s not a minor side effect. That’s enough to make someone unable to stand safely, drive, or even wake up if their breathing slows too much.
What Medications Should You Avoid Mixing With Antihistamines?
Here’s the short list of common medications that become dangerous when paired with first-generation antihistamines:- Benzodiazepines - Xanax, Valium, Ativan, Klonopin
- Opioids - Oxycodone, hydrocodone, codeine, tramadol
- Sleep aids - Zolpidem (Ambien), eszopiclone (Lunesta), zaleplon (Sonata)
- Alcohol - Even one drink can trigger severe drowsiness or respiratory depression
- Muscle relaxers - Cyclobenzaprine (Flexeril), carisoprodol (Soma)
- Some antidepressants - Amitriptyline, trazodone, mirtazapine
- Antipsychotics - Quetiapine (Seroquel), olanzapine (Zyprexa)
It’s not just about the drugs themselves. It’s about the total burden. If you’re taking three medications that each have mild sedating effects, the combination can be deadly. That’s why older adults - who often take multiple prescriptions - are at the highest risk. The American Geriatrics Society has listed diphenhydramine and hydroxyzine on its Beers Criteria as medications to avoid in people over 65, especially if they’re already on other anticholinergic drugs.
Second-Generation Antihistamines Are Safer - But Not Risk-Free
The good news? You don’t have to give up allergy relief. Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) were designed to stay out of the brain. They bind to histamine receptors in the nose and throat, not the central nervous system.Studies show that 97% of people taking loratadine report no drowsiness, compared to 68% with diphenhydramine. In clinical trials, cetirizine showed no significant increase in sedation when taken with benzodiazepines - unlike first-gen antihistamines. That’s why most doctors now recommend these as first-line treatments for allergies.
But here’s the catch: even second-generation antihistamines aren’t completely risk-free. Cetirizine still has a low ACB score of 1. And while it doesn’t cause much sedation on its own, if you’re already taking multiple CNS depressants - say, an opioid plus a sleep aid - adding cetirizine could tip the balance. It’s not the same level of danger as diphenhydramine, but it’s not zero.

What About H2 Blockers Like Tagamet?
You might think, “Wait, isn’t famotidine (Pepcid) an antihistamine too?” Technically, yes - but it works on H2 receptors in the stomach, not H1 receptors in the brain. So it doesn’t cause drowsiness. But there’s another issue: cimetidine (Tagamet), an older H2 blocker, interferes with liver enzymes that break down other drugs.Cimetidine can slow down how quickly your body processes medications like warfarin, theophylline, and even some antidepressants. This can cause those drugs to build up in your system and become toxic. It’s a different kind of interaction - not sedation, but overdose risk. If you’re on any prescription meds and think about switching to Tagamet for heartburn, talk to your pharmacist first.
Real Stories, Real Consequences
Online forums are full of warnings. On Reddit’s r/Pharmacy, a user shared how combining 50mg of Benadryl with 1mg of Xanax led to respiratory failure. They were rushed to the ER. Over 400 similar stories exist in that thread alone.GoodRx users give diphenhydramine a 1.8 out of 5 stars for safety. The top reason? “I took it with my pain meds and couldn’t wake up.” WebMD reports that 41% of people taking diphenhydramine with opioids experienced severe dizziness - more than five times higher than those taking opioids alone.
And it’s not just pills. One user on BuzzRx described a “complete blackout” after one beer and 25mg of Benadryl. That’s less than half the recommended dose. For some people, especially older adults or those with liver problems, even small amounts can be enough to trigger a crisis.
Who’s Most at Risk?
The biggest danger zone is older adults. As we age, our liver and kidneys don’t clear drugs as efficiently. First-generation antihistamines can stick around in the body 50-70% longer in people over 65. That means the sedative effect lasts longer, and the risk of confusion, falls, and delirium skyrockets.A 2021 JAMA Internal Medicine study found that combining diphenhydramine with oxybutynin (a bladder medication) increased delirium risk by 54% in seniors. Another study showed that long-term use of anticholinergics - including diphenhydramine - was linked to a 54% higher risk of dementia.
People with liver disease, chronic kidney disease, or COPD are also at higher risk. Their bodies can’t process these drugs well, so even normal doses can become toxic.
What Should You Do Instead?
If you’re using diphenhydramine as a sleep aid, it’s time to rethink that habit. It’s not designed for long-term use. It disrupts natural sleep cycles and can lead to dependence. For allergies, switch to a second-generation antihistamine. For sleep, try melatonin, good sleep hygiene, or talk to your doctor about safer options like low-dose trazodone - but only if you’re not already on other CNS depressants.Here’s a simple checklist:
- Check every medication you take - even OTC ones - for antihistamine ingredients.
- Look for “diphenhydramine,” “doxylamine,” or “hydroxyzine” on labels.
- Use the Anticholinergic Burden Calculator from the University of Washington to see your total risk.
- If you’re on three or more medications with anticholinergic effects, talk to your doctor about deprescribing.
- Never mix alcohol with any antihistamine, even if it says “non-drowsy.”
What’s Changing in 2026?
The tide is turning. Since 2018, sales of first-generation antihistamines have dropped 12.7% each year. By 2023, second-generation antihistamines made up 83% of the U.S. OTC market. The FDA now requires bold warning labels on diphenhydramine packaging: “May cause severe drowsiness when combined with alcohol, opioids, or sleep medications.”Health systems like Kaiser Permanente have added automated alerts in their electronic records. If a doctor tries to prescribe Benadryl to someone already on an opioid, the system flags it. Since 2020, this has cut antihistamine-related ER visits by 34%.
Newer antihistamines like bilastine and levocetirizine are showing near-zero interaction potential. The future is moving toward medications that target only the receptors they’re meant to - no brain effects, no liver interference, no surprises.
But until then, the safest choice is simple: skip the first-gen antihistamines unless absolutely necessary. And if you’re already taking them with other sedating drugs - talk to your doctor. Don’t wait for a bad reaction to happen.
Can I take Benadryl with my anxiety medication?
No, combining diphenhydramine (Benadryl) with benzodiazepines like Xanax or Ativan is dangerous. This mix can cause extreme drowsiness, slowed breathing, and even loss of consciousness. Even if you’ve done it before without issues, the risk increases with age, liver problems, or higher doses. Switch to a non-sedating antihistamine like loratadine or cetirizine for allergies. For anxiety, work with your doctor to find safer long-term solutions.
Is Zyrtec safer than Benadryl for seniors?
Yes, cetirizine (Zyrtec) is much safer than diphenhydramine for older adults. It doesn’t cross the blood-brain barrier as easily and has a lower anticholinergic burden (ACB score of 1 vs. 3 for Benadryl). However, it’s not completely risk-free - especially if combined with other sedating medications. Still, it’s the preferred choice for allergy relief in seniors. Avoid Benadryl entirely if possible.
Can I use antihistamines as a sleep aid?
It’s not recommended. First-generation antihistamines like diphenhydramine disrupt natural sleep architecture and can cause next-day grogginess, memory issues, and dependence. They’re not designed for long-term use. For insomnia, try melatonin, cognitive behavioral therapy for insomnia (CBT-I), or talk to your doctor about safer prescription options. Don’t rely on allergy meds to help you sleep.
Do all antihistamines cause drowsiness?
No. Only first-generation antihistamines like Benadryl, Unisom, and Phenergan cause significant drowsiness because they enter the brain. Second-generation antihistamines like Claritin, Allegra, and Zyrtec are designed to stay out of the brain and typically don’t cause sedation. However, some people still feel slightly tired on Zyrtec - it’s less common, but possible. Always check the label and start with the lowest dose.
What should I do if I accidentally mixed Benadryl with alcohol?
If you took Benadryl with alcohol and feel extremely drowsy, dizzy, confused, or have trouble breathing, seek medical help immediately. Even if you feel fine, monitor yourself closely for the next 6-8 hours. The effects can build up slowly. Never drive, operate machinery, or go to sleep alone. If you’re over 65 or have health conditions like COPD or liver disease, call your doctor even if symptoms seem mild.






Katie and Nathan Milburn
January 31, 2026 AT 14:06The data presented here is meticulously compiled and aligns with current clinical guidelines on anticholinergic burden. It is imperative that healthcare providers routinely screen for polypharmacy involving first-generation antihistamines, particularly in geriatric populations where pharmacokinetic alterations significantly elevate risk. The 54% increase in dementia correlation is not merely statistical-it represents a preventable public health crisis.
Marc Bains
February 1, 2026 AT 06:31Let’s be real-most people don’t read labels. I’ve seen grandmas take Benadryl with their blood pressure med and think they’re fine because ‘it’s just an allergy pill.’ We need better public education, not just warning labels. Pharmacies should have automated alerts at checkout for OTC meds that interact with common prescriptions. This isn’t just a doctor’s problem-it’s a community one.
kate jones
February 1, 2026 AT 22:16Second-generation antihistamines are the standard of care for a reason. Cetirizine’s ACB score of 1 reflects minimal CNS penetration; loratadine is nearly zero. The misconception that ‘all antihistamines are the same’ persists because of decades of marketing and over-the-counter accessibility. The FDA’s 2023 labeling update is a step forward, but enforcement remains inconsistent. Always verify active ingredients-not brand names. And yes, Zyrtec is still safer than Benadryl for seniors, even with polypharmacy-but monitor for cumulative effects.
Natasha Plebani
February 2, 2026 AT 02:35There’s a deeper philosophical tension here: convenience versus cognitive integrity. We’ve normalized sedation as a solution-to allergies, to insomnia, to anxiety-because it’s easy. But the brain isn’t a machine that can absorb chemical blunt force without consequence. Diphenhydramine doesn’t just cause drowsiness; it erodes the architecture of attention, memory, and self-regulation over time. We treat the symptom, not the system. And in doing so, we trade present comfort for future cognitive erosion. The Beers Criteria isn’t a guideline-it’s a lament.
What if we stopped seeing anticholinergics as ‘harmless sleep aids’ and started seeing them as neurotoxic compromises? The data doesn’t lie. The question is whether we’re willing to face what that means for how we medicate ourselves.
Eliana Botelho
February 2, 2026 AT 17:38Okay but like… I’ve taken Benadryl with wine for years and I’m fine. My grandma took it with Xanax and she’s 82 and still drives. Why are you guys acting like this is some new scary thing? People have been mixing stuff since forever. If you’re scared of side effects, don’t take it. But don’t scare everyone else into thinking every little combo is a death sentence. Also, Zyrtec gives me headaches so I’ll stick with Benadryl thanks.
Rob Webber
February 3, 2026 AT 09:19This article is alarmist nonsense. You’re scaring people into avoiding perfectly legal, over-the-counter medications because of cherry-picked ER stats. People die from falling down stairs too. Should we ban stairs? Benadryl has been used safely for 70 years. The real problem is lazy doctors prescribing opioids and benzodiazepines like candy. Blame the system, not the antihistamine. Also, ‘dementia risk’? That’s correlation, not causation. You’re fueling fear, not facts.
Lisa McCluskey
February 4, 2026 AT 00:53I’m a nurse. I’ve seen the ER results. This isn’t speculation. One patient mixed Benadryl with trazodone and slept for 18 hours, then woke up confused and fell. Broke her hip. No alcohol. No opioids. Just two meds she thought were ‘safe.’ The article is correct. Switch to Claritin. Use melatonin. Talk to your pharmacist. It’s that simple.
owori patrick
February 5, 2026 AT 07:23As someone from Nigeria, I’ve seen this too. People here use diphenhydramine for sleep because it’s cheap and available. No one checks interactions. We need more awareness campaigns in low-resource settings. This isn’t just an American problem-it’s global. Education needs to reach rural clinics and street pharmacies. Thank you for highlighting this.