When a teenager stops eating dinner with the family, skips school, or spends hours in their room with the door locked, it’s easy to brush it off as "just being a teen." But when these signs stick around for weeks - or months - and get worse, it’s not teenage moodiness. It’s depression. And it’s more common than most parents realize. About one in five adolescents in the U.S. will experience a major depressive episode before they turn 18. The good news? There are effective treatments. The hard part? Deciding what’s right for your family.
Family Therapy Isn’t Just "Talking It Out"
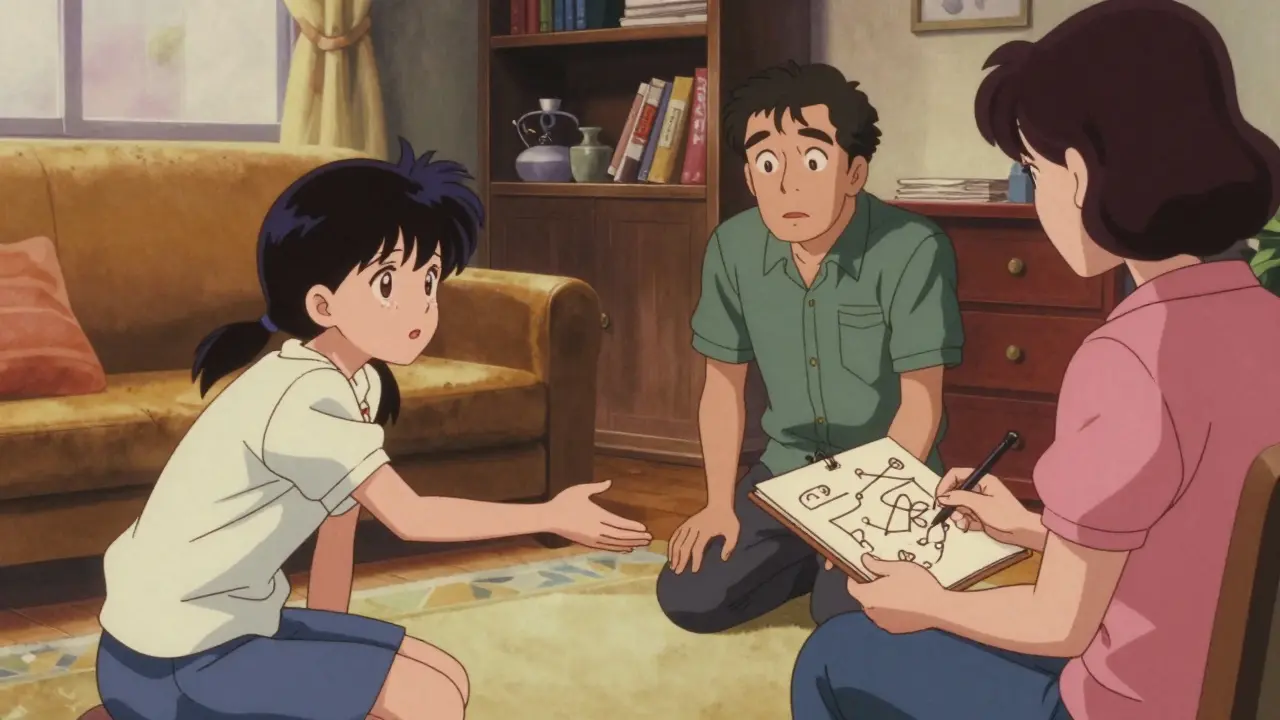
Family therapy for adolescent depression isn’t about blaming parents or forcing everyone to sit in a circle holding hands. It’s a structured, evidence-based approach that treats depression as something shaped by relationships - not just something inside the teen’s head. One of the most proven models is Attachment-Based Family Therapy (ABFT). It targets the emotional disconnect between teens and their caregivers. Think of it like this: when a child feels unsafe expressing sadness, anger, or fear at home, they shut down. That shutdown turns into depression. ABFT helps parents learn how to listen without fixing, validate without judging, and reconnect without pressure. In a 2022 study from Jefferson Digital Commons, teens in ABFT showed significantly lower suicidal thoughts after just 12 weeks compared to those getting standard care. Parents reported fewer arguments, better communication, and a renewed sense of closeness. One mom in Philadelphia told her therapist, "I didn’t realize I was making her feel like her feelings were too much. Now I say, ‘I’m here. Tell me.’ And she does. For the first time in two years." Other family therapy models, like structural and strategic approaches, focus on power dynamics and patterns of conflict. For example, if a teen’s depression keeps the family from arguing about chores, the therapist might gently challenge that unspoken deal. It sounds strange - but sometimes, depression becomes the family’s way of coping. Therapy helps them find healthier ways.Medications: Fast Relief, But Not a Magic Bullet
If depression is severe - if a teen is crying daily, can’t get out of bed, or talks about not wanting to live - therapy alone might not be enough. That’s where medication comes in. The FDA has approved only two antidepressants for teens: fluoxetine (Prozac) and escitalopram (Lexapro). Both are SSRIs, which boost serotonin in the brain. They don’t make someone "happy" overnight. It takes 4 to 6 weeks to feel any change. And during the first few weeks, some teens feel worse - more anxious, restless, or even more suicidal. That’s why doctors require weekly check-ins at first. The Treatment for Adolescents with Depression Study found that 11-18% of teens on SSRIs had what’s called an "activation syndrome" - increased energy, agitation, or impulsivity. That’s why parents need to watch closely. Not every teen reacts the same. Some feel like a fog has lifted. Others get headaches, nausea, or trouble sleeping. About one-third of teens stop taking SSRIs because of side effects. But here’s what most people don’t know: when SSRIs are combined with therapy, the results are stronger. A 2020 review by the Agency for Healthcare Research and Quality showed teens who got both medication and talk therapy improved faster and stayed better longer than those who got just one.Which One Should You Choose? It Depends
There’s no one-size-fits-all answer. But here’s what the data says about who benefits most from each approach:- Choose family therapy if: The teen’s depression is tied to family conflict, emotional neglect, or poor communication. If parents are willing to show up, listen, and change how they interact - this can be life-changing.
- Choose medication if: The teen is severely depressed, has suicidal thoughts, or hasn’t improved after 8-12 weeks of therapy alone. Medication can stabilize mood enough to make therapy more effective.
- Choose both if: The depression is moderate to severe, and the family is open to change. This is the gold standard.
What About Other Options? Exercise, Gratitude, and More
Some parents ask: "Can’t we just try yoga or meditation?" The answer is: yes - but not instead of proven treatments. An eight-week online program based on gratitude and forgiveness showed modest improvements in mood, with no side effects. Regular exercise - even just 30 minutes of walking or biking five days a week - has been shown to reduce depressive symptoms as much as some medications in mild cases. But these work best as supports, not replacements. Digital tools are also emerging. In 2023, the FDA approved the first digital therapeutic for teen depression, called reSET-O. It’s an app that guides users through CBT exercises and syncs with their therapist. Early trials show 72% of teens finish the program when it’s delivered digitally - compared to 58% for in-person therapy.The Real Barrier? Access
Here’s the ugly truth: even if you know what to do, getting help is hard. There are only about 8,500 certified child and adolescent family therapists in the U.S. for 42 million teens. In many areas, the waitlist is 12 to 18 months long. Rural areas are worse - only 19% of teens there receive family therapy, compared to 38% in cities. Insurance doesn’t always cover it well. Some plans only pay for 6 sessions. Others require a diagnosis before approving therapy. And many therapists don’t take insurance at all. The good news? Federal funding is increasing. In 2023, SAMHSA gave $512 million to youth mental health programs - 22% of that went to family-based interventions. The National Institute of Mental Health is expanding ABFT to 15 community centers in 2024, with early results showing a 58% drop in suicidal thoughts after 12 weeks.
What Parents Can Do Right Now
You don’t have to wait for a perfect plan. Here’s what actually helps:- Don’t wait. If your teen shows signs of depression for more than two weeks, talk to their pediatrician. Screening is quick and free under the U.S. Preventive Services Task Force guidelines.
- Ask about therapy first. For mild to moderate depression, start with family therapy. It has no side effects and builds long-term resilience.
- Be ready to participate. Therapy won’t work if you show up but don’t listen. Put your phone away. Say, "I want to understand."
- If meds are suggested, ask questions. What are the risks? How often will we check in? What if side effects happen?
- Use free resources. Call the 988 Suicide & Crisis Lifeline. Visit NAMI.org for parent support groups. Join Reddit’s r/TeenDepression to hear real stories.
What Happens After Treatment?
Depression doesn’t end when the symptoms fade. Half of teens who recover will have another episode within five years. That’s why the American Academy of Pediatrics recommends monthly check-ins for up to two years after remission. The goal isn’t just to feel better. It’s to build a family that can handle hard times - together.Is family therapy effective for teen depression?
Yes, especially for teens whose depression is tied to family conflict or emotional distance. Attachment-Based Family Therapy (ABFT) has shown strong results in reducing suicidal thoughts and improving communication. A 2022 study found teens in ABFT improved more than those in standard care. It works best when parents are willing to change how they interact.
Are antidepressants safe for teenagers?
Fluoxetine (Prozac) and escitalopram (Lexapro) are the only two antidepressants FDA-approved for teens. They’re generally safe when monitored closely. But in the first few weeks, some teens experience increased anxiety or suicidal thoughts - which is why weekly check-ins with a doctor are required. About one-third of teens stop taking them due to side effects like nausea, headaches, or insomnia. Never stop medication suddenly.
Can my teen get better without medication?
Yes - many teens recover with therapy alone, especially if the depression is mild to moderate and the family is engaged. Family therapy, cognitive behavioral therapy (CBT), and even regular exercise can be enough. But if symptoms are severe - like constant crying, skipping school, or talking about death - medication combined with therapy is often the fastest and most effective path.
How long does family therapy take?
Most family therapy programs last 12 to 16 weeks, with weekly 50- to 90-minute sessions. Attachment-Based Family Therapy usually takes longer - 16 to 20 sessions - because it focuses on deep emotional repair. Structural or strategic therapy may show results faster, in 8 to 10 sessions. Progress depends on family participation, not just time.
What if my teen refuses to go to therapy?
Start with the parents. Many family therapy models allow parents to attend sessions alone at first. Therapists can help you learn how to talk differently, set boundaries, and create a calmer home. Often, when parents change their approach, the teen starts to open up on their own. Some therapists also offer virtual sessions or teen-only check-ins to build trust before bringing everyone together.
Is family therapy covered by insurance?
Many insurance plans cover family therapy under mental health benefits, but coverage varies. Some limit the number of sessions. Others require a diagnosis. Call your insurer and ask: "Does my plan cover MFT (Marriage and Family Therapy) for adolescent depression?" If not, ask your pediatrician for low-cost clinics or community mental health centers. SAMHSA’s National Helpline (1-800-662-4357) can help you find free or sliding-scale options.
What’s the biggest mistake parents make?
Trying to fix it instead of listening. Many parents jump in with advice: "Just get more sleep," "Stop being so sensitive," or "You have so much to be grateful for." These responses, even when well-meaning, make teens feel misunderstood. The most powerful thing you can say is: "I see you’re hurting. I’m here. I don’t have to fix it - I just want to understand."
Depression in teens doesn’t vanish because you wish it would. But it doesn’t have to define their future either. With the right support - whether it’s therapy, medication, or both - most teens find their way back. The key isn’t perfection. It’s presence.






Nat Young
January 14, 2026 AT 21:49Let’s be real - family therapy is just a fancy way to make parents feel better while the kid keeps spiraling. ABFT? More like ABF*Wait-And-See*. The data’s cherry-picked. I’ve seen teens in therapy for a year and still skip school, still delete texts, still sleep 14 hours a day. Meanwhile, SSRIs? Yeah, the first few weeks suck - but after that? A kid who couldn’t get out of bed starts doing homework. That’s not magic. That’s neurochemistry.
Iona Jane
January 15, 2026 AT 09:23They don’t want you to know this but SSRIs are part of a Big Pharma plot to chemically neuter teens so they stop questioning authority. The FDA approved them because the same people who fund the studies also own the drug patents. And family therapy? That’s just social engineering - training kids to be obedient little emotional sponges for their traumatized parents. You think your kid’s depressed? Maybe they’re just awake. The system is rigged.
Jaspreet Kaur Chana
January 17, 2026 AT 07:24Bro in India we got nothing like this. No therapists, no insurance, no Prozac in rural towns. My cousin’s 16-year-old daughter cried every night for six months and her mom just said ‘beta, tumhara dimaag kharab hai’ - your brain is broken. We don’t have ABFT, we have chai, silence, and prayer. But here’s the thing - when my uncle started cooking her favorite dal every night and sat with her without saying a word? She started talking. Not because of therapy. Because someone finally stopped trying to fix her and just stayed. Sometimes love is the only evidence-based treatment we’ve got.
Haley Graves
January 17, 2026 AT 22:39Parents: stop waiting for the perfect solution. Start with one thing. Ask your teen what they need. Not ‘do you want therapy?’ - ask ‘what would make today feel a little less heavy?’ If they say nothing, sit with them in silence for five minutes. Then do it again tomorrow. That’s not therapy. That’s presence. And presence is the first step to healing - no prescription needed.
Nilesh Khedekar
January 18, 2026 AT 04:13Wait - you’re telling me a 16-year-old who’s been ignored for years can just ‘reconnect’ with a 12-week therapy program? That’s like expecting a cracked foundation to fix itself after a coat of paint. And SSRIs? Sure, they work - for the 20% who don’t get suicidal ideation or weight gain or emotional numbness. Meanwhile, the other 80% are just medicated zombies trying to pass algebra. And don’t even get me started on ‘digital therapeutics’ - now we’re outsourcing mental health to apps? Next they’ll sell depression patches on Amazon.
Niki Van den Bossche
January 18, 2026 AT 05:55The entire paradigm is fundamentally flawed. You’re treating depression as a clinical entity rather than an existential rupture - a metaphysical collapse born of late-stage capitalism, algorithmic alienation, and the collapse of intergenerational meaning. Family therapy? It’s just bourgeois emotional labor. Medication? A pharmacological pacifier for the disenchanted. The real cure? A radical re-embedding of the adolescent into a mythic, communal narrative - not CBT, not ABFT, not SSRIs - but a return to ritual, to silence, to ancestral witnessing. But of course, you’d rather pay for a 90-minute session with a licensed therapist who’s never read Heidegger.
Jan Hess
January 19, 2026 AT 01:38I’ve been in both camps - therapy and meds. I started with therapy but my parents kept saying ‘we’re here for you’ while scrolling TikTok during sessions. Then I got Prozac. First two weeks I wanted to jump off a bridge. Fourth week? I laughed at a meme for the first time in a year. Didn’t fix everything. But it gave me the energy to show up for therapy. So yeah - both. Not either/or. Both.
Gloria Montero Puertas
January 19, 2026 AT 22:01Let’s be honest - if your kid is depressed, you probably raised them wrong. You gave them too much screen time, too little discipline, too many trophies for showing up. Now you want a pill or a hug session to fix it? Newsflash: depression isn’t trauma porn. It’s a consequence of weak parenting. Stop outsourcing your responsibility to therapists and psychiatrists. Go home. Set boundaries. Make them earn their phone back. Discipline. Structure. Love. Not ‘validation.’
Frank Geurts
January 20, 2026 AT 17:30While the data presented is statistically significant and methodologically sound, it is imperative to acknowledge the structural limitations inherent in the American mental healthcare infrastructure. The scarcity of certified child and adolescent family therapists - approximately 8,500 for a population of 42 million adolescents - constitutes a systemic failure of public policy. Furthermore, the disparity in access between urban and rural communities, coupled with inconsistent insurance reimbursement protocols, suggests that the efficacy of evidence-based interventions is contingent not upon clinical merit, but upon socioeconomic privilege. This is not a medical issue. It is a moral one.
Annie Choi
January 22, 2026 AT 11:30Y’all are overcomplicating this. The real issue? Access. Not whether ABFT works. Not whether Lexapro’s safe. Can you even get an appointment? In my town, the waitlist for a child therapist is 14 months. Meanwhile, the kid’s failing classes, self-harming, and the school counselor says ‘just try yoga.’ We need crisis teams in schools. We need telehealth subsidies. We need insurance to cover 20 sessions - not 6. Stop debating the gold standard when most families can’t even get to the starting line.
Arjun Seth
January 23, 2026 AT 21:13Medication is sin. Depression is a spirit problem. Your kid is not broken - they’re possessed by laziness and disobedience. I’ve seen it. My nephew stopped crying after I made him wake up at 5 AM, pray for an hour, and clean the whole house. No pills. No therapy. Just discipline. God doesn’t want your kid on antidepressants. He wants your kid to get up and work. Stop coddling them. Sin causes depression. Repentance fixes it.
Dan Mack
January 25, 2026 AT 18:43ABFT is a cult. The therapist tells parents to say ‘I’m here’ and suddenly everything’s fixed? What if the kid hates them? What if the mom was the one who abused them? What if the dad left? What if the family is toxic and the therapy just makes them pretend it’s not? You think therapy heals trauma? Nah. It just makes people say nice things while the wounds fester. And SSRIs? They’re just chemical tranquilizers for a society that refuses to fix the real problems.
Amy Vickberg
January 26, 2026 AT 10:19My daughter started therapy at 15. We did ABFT. First session, I cried because I realized I’d been asking ‘what’s wrong with you?’ instead of ‘what happened to you?’ It took 16 weeks. She didn’t magically become happy. But she started eating dinner with us again. She told me she didn’t want to die. That’s not a statistic. That’s my daughter. If you’re scared to try therapy because you think you’ll fail - good. That means you care. Show up anyway.
Ayush Pareek
January 28, 2026 AT 05:30For those in India or anywhere with no access - don’t wait. Walk with your kid. No advice. Just walk. Morning or night, doesn’t matter. Talk about nothing. The sky. The road. The dog next door. Silence is okay. After a week, they’ll start talking. Not because you fixed anything. Because you showed up. That’s all they need. Not a therapist. Not a pill. Just you.
Nishant Garg
January 29, 2026 AT 15:18Here’s the truth nobody wants to admit: therapy works if your family isn’t a warzone. Medication works if you’ve got a doctor who actually listens. But if you’re poor, brown, or live in a town with no mental health services? You’re screwed. And the system knows it. They write these beautiful articles for middle-class parents who can afford $200 sessions and insurance that covers 12 visits. Meanwhile, my cousin’s kid took a 3-hour bus ride to the nearest clinic - and got a pamphlet. That’s not healthcare. That’s a cruel joke dressed up as hope.