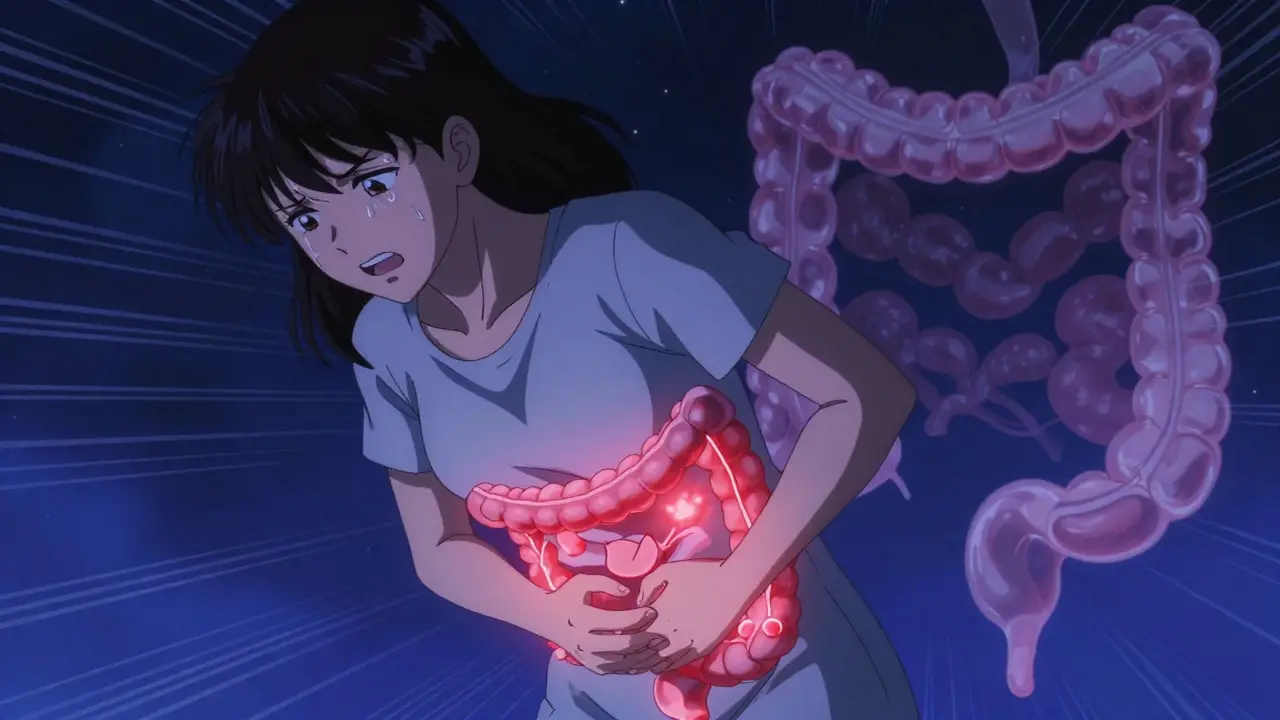
When your lower left abdomen suddenly feels like it’s being stabbed with a hot knife, and you can’t stand up straight, it’s not just gas. It could be diverticulitis-inflammation of small pouches in your colon that shouldn’t be irritated. This isn’t rare. Nearly 6 in 10 Americans over 60 have these pouches, called diverticula. Most never cause trouble. But when they get infected or inflamed, things turn serious fast.
What Exactly Are Diverticula?
Diverticula are tiny bulges, usually 5 to 10 millimeters wide, that stick out from the wall of your colon. Think of them like weak spots in a balloon that puff out under pressure. They form because the muscle layer in your colon gets strained over time, often from low-fiber diets and chronic constipation. The pressure builds, and the inner lining pushes through the thin spots. About 95% of these pouches appear in the sigmoid colon-the S-shaped part near the end of your large intestine. That’s why most people feel pain on the lower left side.Having diverticula without inflammation is called diverticulosis. It’s common, especially as you age. But when bacteria get trapped inside one of those pouches, or when a small piece of stool blocks it, inflammation kicks in. That’s diverticulitis. It’s not just discomfort-it’s an infection that can spread if not handled right.
How Do You Know It’s Diverticulitis and Not Something Else?
Many people mistake diverticulitis for IBS, appendicitis, or even a urinary tract infection. But there are clear signs that set it apart:- Sharp, constant pain in the lower left abdomen (right-sided pain happens in up to 40% of Asian patients)
- Fever above 38°C (100.4°F)
- Nausea or vomiting
- Changes in bowel habits-constipation or diarrhea
- Leukocytosis (high white blood cell count)
Unlike IBS, where pain comes and goes and isn’t tied to fever, diverticulitis pain usually gets worse with movement. You might find yourself leaning forward or curling up because standing straight hurts too much. If you’ve had this before, you know the difference. But if it’s your first time, you might end up in the ER thinking it’s a kidney stone or ovarian cyst-especially if you’re a woman. Studies show about 25% of cases are misdiagnosed at first.
The gold standard for diagnosis is a CT scan. It shows exactly where the inflammation is and how bad it is. Doctors use the Hinchey system to classify severity:
- Stage Ia: Small abscess near the colon
- Stage Ib: Larger abscess, still contained
- Stage II: Abscess in the pelvis
- Stage III: Pus spreading into the abdominal cavity
- Stage IV: Fecal leakage into the belly-this is an emergency
Stage I and II are often treated without surgery. Stage III and IV? That’s when you need a surgeon right away.
Antibiotics: Still Necessary?
Ten years ago, every case of diverticulitis got antibiotics. Now? Not so much.Big studies like the 2021 DIVERT trial found no difference in recovery time between people who took antibiotics and those who didn’t-when the case was mild. If you’re otherwise healthy, have no fever, and your blood work looks normal, your doctor might just tell you to rest, drink fluids, and eat clear liquids for a couple of days.
But here’s the catch: If you have a fever over 38.5°C, your white blood cell count is sky-high, or you’re feeling really sick, antibiotics are still needed. The goal isn’t to kill every single case-it’s to stop the infection before it spreads. Common choices include amoxicillin-clavulanate (Augmentin) or ciprofloxacin with metronidazole. For hospital cases, IV antibiotics like piperacillin-tazobactam are used.
One big shift? Doctors no longer recommend antibiotics for everyone. That’s because overuse leads to resistant bacteria and gut damage. The American Gastroenterological Association updated its guidelines in 2023 to reflect this. It’s not about fear-it’s about smart treatment.
What to Eat When You’re Flaring Up-and After
For the first 48 to 72 hours of a flare-up, you’ll likely be on a clear liquid diet: water, broth, gelatin, apple juice. No solids. Your colon needs to rest.Then, you slowly move to low-fiber foods: white bread, eggs, cooked chicken, mashed potatoes, canned peaches. No raw veggies, nuts, seeds, or whole grains yet. This lasts about a week.
Once you’re feeling better, the real key kicks in: fiber. Not just any fiber-25 to 35 grams a day. That’s a big jump for most people. One cup of lentils has 15 grams. One cup of cooked oats has 4. So you need variety: beans, berries, chia seeds, whole grains, broccoli.
And yes, you heard right-nuts and seeds are safe. For decades, doctors told people to avoid them. But a 18-year study of 47,000 women found no link between eating nuts, popcorn, or seeds and getting diverticulitis. In fact, those who ate them regularly had lower rates of attacks.
High fiber isn’t just prevention-it’s protection. One patient on MyCrohnsAndColitisTeam said after increasing fiber to 35g daily, he went 27 months without another flare. That’s not luck. That’s science.
When Surgery Becomes an Option
Most people never need surgery. But if you’ve had two or more attacks that landed you in the hospital, your doctor might bring it up. Why? Because between flares, many people live with constant discomfort-bloating, cramping, fear of the next attack. Quality of life drops.Old guidelines said wait for three attacks. Now, the American Society of Colon and Rectal Surgeons says: consider surgery after two hospitalizations. The goal isn’t to remove your colon-it’s to remove the part that keeps causing trouble. Usually, that’s the sigmoid colon.
Two main procedures:
- Laparoscopic lavage: Drain the infection and clean the area. Works well for Stage III if the leak is contained.
- Resection: Remove the damaged section and reconnect the healthy parts. More permanent, but more invasive.
The 2022 SCANDIV trial showed laparoscopic lavage worked in 82% of cases, compared to 67% for immediate resection. But resection has lower recurrence rates long-term. It’s a trade-off: less surgery now versus lower risk of future attacks.
What Happens After the Attack?
Once you’re better, you’ll need a colonoscopy. Not because you have cancer-but because diverticulitis can hide it.A 2021 JAMA study found that 1.3% of people over 50 who had diverticulitis also had colon cancer. That’s not high, but it’s enough to warrant checking. The colonoscopy is usually done 6 to 8 weeks after the flare settles. Why wait? Because inflammation makes it hard to see clearly. Wait until things calm down.
And if you’re over 50 and haven’t had a colonoscopy yet? Get one. Diverticulitis is a wake-up call.

New Treatments on the Horizon
The future of diverticulitis care isn’t just about antibiotics and surgery. It’s about prevention and precision.In 2023, the FDA approved mesalazine (Pentasa) for maintenance therapy. In a trial called DIVA-2, patients who took it daily had a 31% lower chance of another attack over 12 months. It’s not a cure, but it’s a tool.
Researchers are also looking at the gut microbiome. People who get frequent attacks have much lower levels of Faecalibacterium prausnitzii, a good bacteria that reduces inflammation. Future treatments might include targeted probiotics or even fecal transplants.
And AI is stepping in. Mayo Clinic built an algorithm that looks at your CT scan, blood tests, age, and BMI to predict your risk of another attack-with 83% accuracy. That means doctors can now say: “You’re at high risk. Let’s start fiber and mesalazine now.”
Who’s at Risk-and What You Can Do
Diverticulitis isn’t just an “old person’s disease.” More than 20% of hospitalizations now happen in people under 44. Why? Three big reasons:- Obesity: A BMI over 30 doubles your risk.
- Smoking: Smokers are 2.7 times more likely to get it.
- Sitting too much: People who exercise less than 2 hours a week have 38% higher incidence.
And yes, stress plays a role too-not directly, but because it affects digestion and eating habits. Fast food, processed carbs, and low water intake? That’s the perfect storm.
The fix? Simple, but not easy:
- Get 25-35g of fiber daily
- Drink 2-3 liters of water
- Move at least 30 minutes a day
- Quit smoking
- Don’t ignore chronic constipation
It’s not glamorous. But it works. And it’s cheaper than emergency surgery.
What to Do If You Think You Have It
If you’re having sudden, severe pain in your lower left abdomen, especially with fever or vomiting:- Don’t take NSAIDs like ibuprofen-they raise the risk of perforation.
- Use acetaminophen (Tylenol) for pain if needed.
- Don’t eat solid food until you’ve been evaluated.
- Call your doctor or go to urgent care. Don’t wait.
Most cases can be handled outpatient. But if you’re in too much pain to walk, have a high fever, or feel dizzy, go to the ER. Delaying care can turn a mild case into a life-threatening one.
Diverticulitis is manageable. It’s not a death sentence. But it’s a signal. Your colon is telling you something’s off. Listen to it.
Can diverticulitis go away without antibiotics?
Yes, for mild, uncomplicated cases. Studies show that people who rest, hydrate, and eat a clear liquid diet often recover just as well as those who take antibiotics. Antibiotics are now reserved for cases with fever, high white blood cell count, or signs of spreading infection.
Is it safe to eat nuts and seeds if I have diverticulitis?
Yes. Older advice told people to avoid nuts, seeds, and popcorn, but large studies-including an 18-year analysis of 47,000 women-found no link between these foods and flare-ups. In fact, eating them may lower your risk. After recovery, they’re part of a healthy high-fiber diet.
How long does a diverticulitis flare last?
Mild cases usually improve within 5 to 7 days with rest and diet changes. If antibiotics are needed, you’ll take them for 7 to 10 days. Hospitalized cases may take 10 to 14 days to resolve. Full recovery to a normal diet can take 2 to 4 weeks.
Can diverticulitis come back?
Yes. Between 15% and 30% of people have another attack after their first. Risk goes up with obesity, smoking, low fiber, and lack of exercise. Taking mesalazine and increasing fiber intake can cut recurrence by up to 31%.
Do I need a colonoscopy after diverticulitis?
Yes, if you’re over 50 or haven’t had one recently. Diverticulitis can mask colon cancer. A colonoscopy 6 to 8 weeks after your flare clears helps rule out tumors. Even though cancer is found in only about 1.3% of cases, it’s worth checking.
When should I consider surgery for diverticulitis?
Surgery is now considered after two hospitalizations for diverticulitis, not three. If you’re having frequent attacks, constant pain between flares, or complications like abscesses, surgery to remove the affected part of the colon (usually the sigmoid) can improve your quality of life and prevent emergencies.






Martin Viau
January 2, 2026 AT 01:19Let’s be real-this article reads like a pharmaceutical whitepaper dressed up as a Reddit post. Antibiotics? Overused. Fiber? Obvious. But nobody talks about how the American diet is just a slow-motion colon suicide pact. We eat processed garbage, sit all day, and then act shocked when our guts revolt. Meanwhile, Canada’s healthcare system is still laughing at how we treat this like a mystery instead of a predictable consequence of capitalism’s food industrial complex.
Marilyn Ferrera
January 2, 2026 AT 12:56Diverticulitis isn’t a disease-it’s a symptom. A symptom of chronic dehydration, low fiber, and emotional stress disguised as convenience. The body doesn’t lie. When your colon screams, it’s not being dramatic-it’s begging you to listen. Fiber isn’t optional. Water isn’t a suggestion. Movement isn’t a trend. These aren’t hacks-they’re biological necessities.
Harriet Hollingsworth
January 2, 2026 AT 14:40So let me get this straight-you’re telling me people still believe nuts cause diverticulitis? Like, in 2024? Who’s still teaching this? It’s 2024. We have peer-reviewed studies. We have data. And yet, people still cling to 1970s dietary myths like they’re gospel. This is why medicine is broken. We prioritize tradition over truth. And it’s killing people. Slowly. Quietly. And with way too much bureaucracy.
Deepika D
January 3, 2026 AT 19:01Hey everyone-I’ve been living with diverticulosis for 12 years, and I want to say: you’re not alone. I used to be terrified of every twinge. Then I learned: it’s not about perfection, it’s about consistency. I started with one cup of lentils a day-just one. Then added chia seeds. Then moved to oatmeal with berries. I didn’t go from zero to hero overnight. I went from ‘I’m scared to eat’ to ‘I know my body now.’ And guess what? I haven’t had a flare in 4 years. It’s not magic. It’s just showing up. Every day. Even when you don’t feel like it. Even when you’re tired. Even when you want pizza. You do it anyway. Because your colon deserves respect. And you? You deserve to feel good.
Bennett Ryynanen
January 5, 2026 AT 06:55Bro. I had this last year. Thought it was a kidney stone. Ended up in the ER with a fever of 101.5. They gave me cipro and metronidazole. Told me to eat broth for three days. I did. And I’m still alive. But here’s the real deal: I didn’t change my diet after. Guess what? Came back six months later. This time? I’m done playing. I’m eating beans, drinking water like it’s my job, and walking after dinner. No more ‘I’ll start Monday.’ Monday’s here. And I’m not waiting again.
Chandreson Chandreas
January 6, 2026 AT 09:15Man… this hits different. 😔 I’m 38, live in Delhi, eat mostly rice and fried stuff. Never thought about fiber until I got this. Now I’m eating oats, flax, and apples like they’re my new best friends. Still mess up sometimes-but I’m trying. Thanks for the info. 🙏 You guys are the real MVPs.
Darren Pearson
January 6, 2026 AT 10:38While the article presents a reasonably comprehensive overview of diverticulitis management, it lacks a critical discussion regarding the socioeconomic determinants of dietary adherence. The recommendation to consume 35 grams of fiber daily is, in practice, inaccessible to populations reliant on processed food subsidies and food deserts. One cannot ethically prescribe nutritional interventions without acknowledging structural inequities in access. Furthermore, the normalization of surgical intervention as a quality-of-life solution warrants deeper bioethical scrutiny.
Stewart Smith
January 7, 2026 AT 13:38So… you’re telling me the cure for my colon’s drama is… more broccoli? And walking? Wow. What a revolutionary idea. Next you’ll tell me breathing oxygen helps. 😏
Aaron Bales
January 8, 2026 AT 16:11Don’t skip the colonoscopy. Even if you feel fine. One in 77 people over 50 with diverticulitis have hidden cancer. That’s not a gamble. That’s a medical obligation. Get it done. No excuses.
Brandon Boyd
January 9, 2026 AT 15:48You got this. I know it feels overwhelming-fiber, water, walking, quitting smoking, all at once. But pick one. Just one. Do it for a week. Then add another. You don’t have to fix everything today. You just have to start. And if you slip? That’s okay. Tomorrow’s a new day. Your body isn’t mad at you. It’s just asking you to show up. And you? You’re already doing better than you think.