It’s not rare to walk out of the pharmacy with a prescription in hand, read the label, and think: Wait, what does this actually mean? You’re not alone. Millions of Americans take at least one medication every day. One in four takes three or more. And yet, confusing instructions are one of the biggest reasons people take pills the wrong way-leading to side effects, hospital visits, or worse.
Why Medication Instructions Are So Hard to Understand
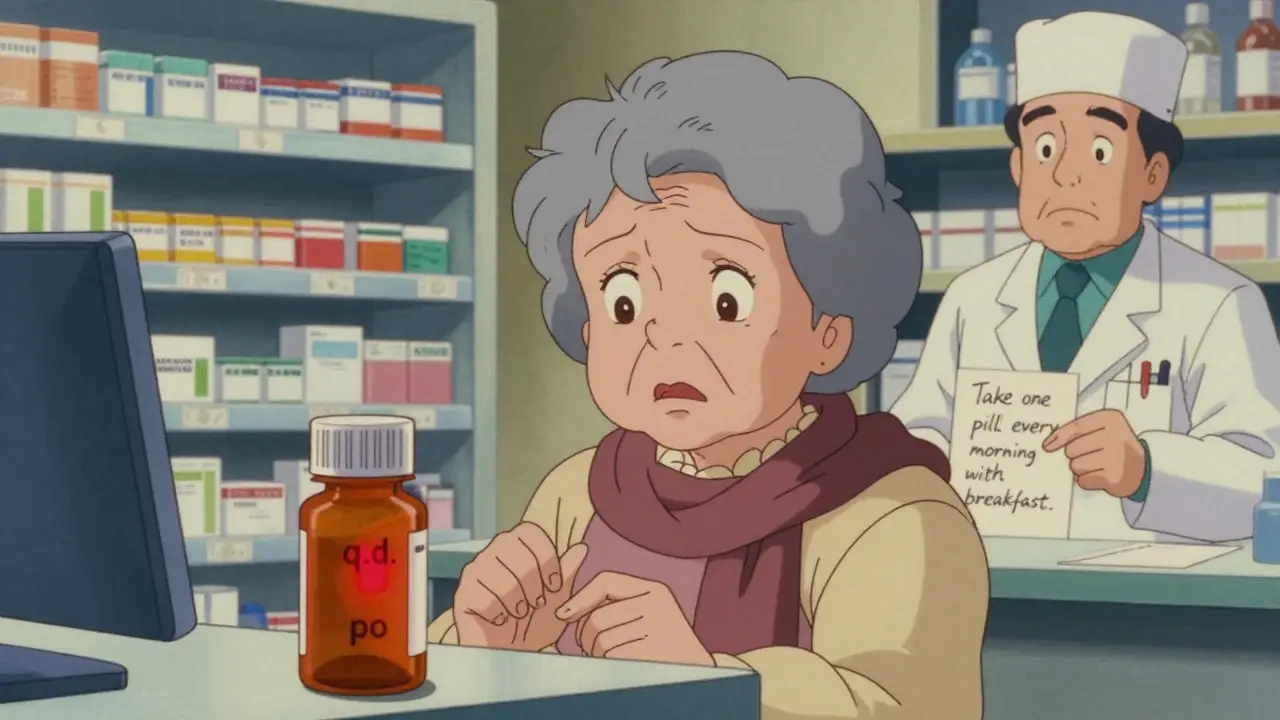
Pharmacies and doctors don’t set out to confuse you. But the system is full of shortcuts that sound fine to professionals but make no sense to patients. You might see things like:- "Take q.d." - That’s Latin for "once daily," but most people don’t know Latin.
- "IN" - Could mean intranasal (through the nose), but looks like IV (intravenous) or IM (intramuscular).
- "1 tab po q am" - "po" means by mouth, "q am" means every morning. But if you don’t know the abbreviations, it’s just gibberish.
- "Take as needed" - Does that mean once a day? Three times? Only when you’re in pain? What’s the max per day?
What the FDA and Other Agencies Say About Clear Instructions
The U.S. Food and Drug Administration (FDA) started requiring Medication Guides back in 1998 for drugs with serious risks-like opioids, isotretinoin (Accutane), or birth control pills. These are printed handouts you get when you pick up the prescription. They explain the risks, what to watch for, and how to take the drug safely. But here’s the catch: Medication Guides are only required for about 200 high-risk drugs. For the thousands of other medications you take-antibiotics, blood pressure pills, thyroid meds-there’s no legal requirement for a printed guide. That’s where the confusion starts. Even worse, different manufacturers of the same generic drug can give different instructions. One company says to take a pill with food. Another says take it on an empty stomach. One says twice daily at 8 a.m. and 8 p.m. Another says "every 12 hours." If you switch brands and don’t notice the difference, you could be taking it wrong. The National Institutes of Health (NIH) says doctors and pharmacists should compare instructions from all manufacturers when prescribing or dispensing. But in practice? That rarely happens unless you ask.How to Ask for Clarification Without Feeling Awkward
You don’t need to be a medical expert to understand your own meds. Here’s exactly what to say:- "Can you walk me through how to take this? I want to make sure I get it right."
- "What does 'as needed' mean for this pill? How many times a day is safe?"
- "Is there a specific time I should take this? Like with food, or before bed?"
- "I’ve taken this before, but the label looks different. Did something change?"
- "Can you write it down in plain English? Like, 'Take one pill every morning with breakfast' instead of '1 tab po q am'?"
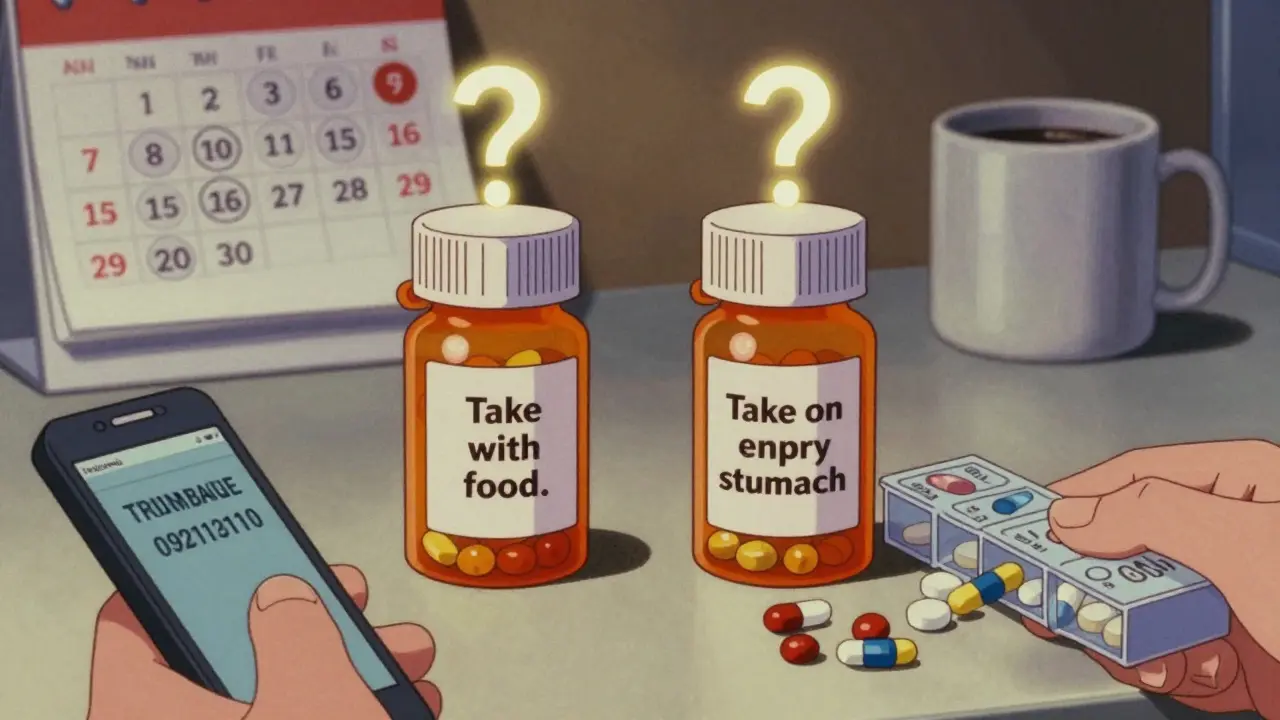
What to Do When Instructions Conflict Between Brands
Say you’ve been taking a generic version of a drug for months. Your insurance switches you to a different generic. The new bottle says: "Take on an empty stomach." The old one said: "Take with food." Don’t guess. Don’t assume they’re the same. Call your doctor or pharmacist. Ask: "Are these two versions of the same drug supposed to be taken differently?" Sometimes the difference matters. For example, some cholesterol-lowering drugs work better when taken at bedtime because your body makes more cholesterol overnight. If you suddenly switch from morning to night without knowing why, you might not get the full benefit. The NIH recommends that prescribers review instructions from all manufacturers when there’s a mismatch. But if they don’t catch it, you have to be the one to speak up.Practical Tips to Avoid Mistakes
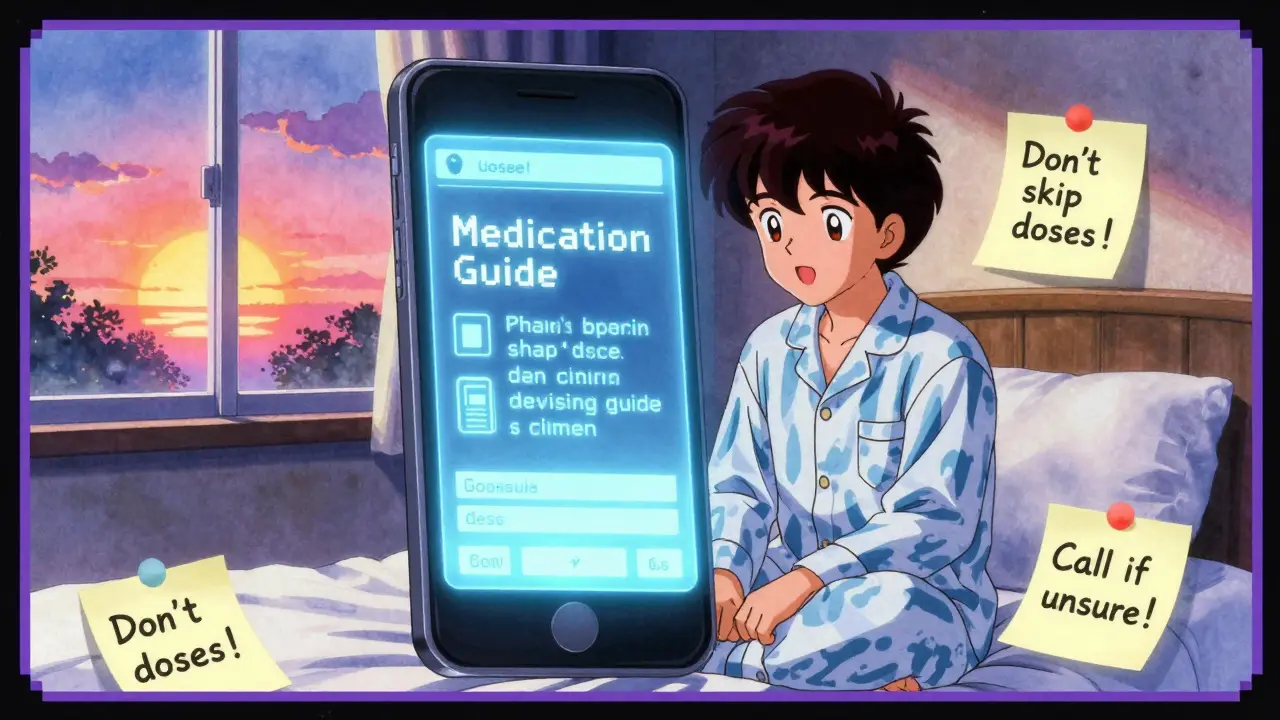
Here are simple, real-world steps you can take right now:- Keep a written list of every medication you take, including the dose and timing. Update it every time something changes.
- Use a pill organizer with labeled compartments for morning, afternoon, evening, and bedtime.
- Set phone alarms for pills that need to be taken at specific times-like every 12 hours. Don’t rely on memory.
- When you get a new prescription, ask the pharmacist: "Is there a Medication Guide for this?" If they say no, ask why-and if you can get one anyway.
- Don’t trust the pharmacy label alone. Compare it to the written instructions your doctor gave you. If they don’t match, call the doctor’s office.
What to Do If You’ve Already Taken a Pill Wrong
If you realize you took a pill at the wrong time, skipped a dose, or took too much, don’t panic-but don’t ignore it either. Call your pharmacist. They’re trained to handle these situations. They can tell you:- Whether it’s safe to take the next dose on schedule
- If you need to skip a dose
- What symptoms to watch for
- When to go to urgent care or the ER






Trevor Davis
January 12, 2026 AT 19:09I used to just swallow pills like candy until my grandma ended up in the ER because she thought 'q.d.' meant 'whenever I remember.' Now I always ask the pharmacist to write it out in plain English. Seriously, if they can't explain it to a 70-year-old, the label is broken.
It's not my job to decode Latin. It's theirs to make it clear.
Damario Brown
January 13, 2026 AT 05:29lol this whole post is just ‘ask more’ but nobody talks about how pharmacies are understaffed and rushed. I’ve had pharmacists scream at me for asking what ‘po’ means. Like, it’s literally on the bottle. Why do I have to be the one to fix your systemic laziness?
Also, generic brands changing instructions without telling you? That’s not negligence, that’s corporate fraud. Someone should sue.
And don’t even get me started on how the FDA only cares about ‘high-risk’ drugs. My blood pressure med almost killed me because the label said ‘take with food’ and the new batch said ‘take on empty stomach.’ No one caught it. Not my doc, not the pharmacist. I had to Google it at 2 a.m.
Priyanka Kumari
January 14, 2026 AT 00:47Thank you for writing this. As someone who helps elderly relatives navigate medications across India and the US, I can say this issue is global. In my village, people take antibiotics until they feel better - not because they’re stubborn, but because the instructions were never explained.
Simple solutions work: write the schedule on a sticky note, use a pill box, and never be afraid to say, ‘Can you say that again like I’m five?’
Healthcare shouldn’t require a degree to understand. You deserve clarity. Keep asking. You’re not being difficult - you’re being brave.
Avneet Singh
January 15, 2026 AT 14:22How quaint. The real problem isn’t ambiguous labeling - it’s the cognitive decline of the American public. If you can’t parse basic medical abbreviations, maybe you shouldn’t be managing polypharmacy at all. The system isn’t broken; it’s filtering out the incompetent.
Also, ‘q.d.’ isn’t Latin - it’s Latin-derived medical shorthand. You wouldn’t ask a chef to explain what ‘mise en place’ means. Why should pharmacists dumb down their lexicon for the untrained?
Perhaps the solution is not clearer labels, but better public education. Or maybe just don’t take so many pills.
Adam Vella
January 16, 2026 AT 23:22One cannot help but observe the profound epistemological rupture between the medical establishment’s symbolic language and the lived experience of the layperson. The use of Latin abbreviations - relics of a pre-Enlightenment medical tradition - persists not out of necessity, but out of institutional inertia.
There is a moral imperative here: if a system of communication is designed to exclude, it is not a system of care - it is a system of control. The FDA’s minimalistic approach to Medication Guides reveals a deeper pathology: the commodification of health as a transaction, not a relationship.
Clarification is not a favor. It is a right. And until the state enforces plain-language standards across all pharmaceutical labeling - not just ‘high-risk’ drugs - we are complicit in systemic harm.
vishnu priyanka
January 17, 2026 AT 19:05Man, this hit different. In India, we got this thing called ‘dadi ka nuskha’ - grandma’s recipe. People mix pills with tea, take them with milk, skip doses because ‘it’s just a headache pill.’ No one reads the label. But here’s the twist - they’re fine. Mostly.
Still, I get it. My cousin took his diabetes med wrong for six months because the bottle said ‘once daily’ but the script said ‘twice.’ No one told him.
Maybe the real fix isn’t labels - it’s culture. Talk about meds like you talk about your favorite food. No shame. Just ask.
Alan Lin
January 19, 2026 AT 02:58Let me be unequivocally clear: this is not a matter of personal responsibility. It is a public health emergency. The fact that 1.5 million preventable injuries occur annually due to ambiguous labeling is not an accident - it is a failure of governance, corporate accountability, and professional ethics.
Pharmacists are not merely dispensers; they are gatekeepers of safety. If they are unwilling or unable to communicate clearly, they are failing their oath. Institutions that permit this are complicit.
Do not ‘ask more.’ Demand more. File complaints. Contact your state board of pharmacy. Write to your representatives. This is not about being ‘awkward’ - it is about survival. And if you are reading this and thinking, ‘I’m too busy to ask,’ then you are already part of the problem.
Pankaj Singh
January 19, 2026 AT 11:25Everyone’s acting like this is some new problem. Newsflash: pharmacists have been lazy since the 80s. You think ‘q.d.’ is confusing? Try reading handwritten scripts from the 90s. I’ve seen ‘take 2’ written as ‘take 20’ - and people died.
Stop pretending this is about language. It’s about accountability. No one’s getting fired for mislabeling. No one’s getting fined. So why would they care?
And don’t even get me started on generic brands. One company’s ‘every 12 hours’ is another’s ‘twice daily.’ They’re not even the same drug in practice. The FDA should ban generics unless they match the brand’s dosing exactly. End of story.
Scottie Baker
January 20, 2026 AT 13:54Bro, I took my thyroid med with coffee for a year because the label said ‘take on empty stomach’ and I thought that meant ‘don’t eat after.’ Turns out it meant ‘don’t eat before.’ I was literally poisoning myself.
Now I screenshot every label, text it to my sister, and ask her if it makes sense. She’s not a nurse - she’s just not dumb.
Don’t be a hero. Don’t guess. Text someone. Call the pharmacy. Even if it’s 11 p.m. They’ve heard it all. And honestly? They’d rather you ask than end up on the news.