Why Medication Regimens Get Too Complicated for Older Adults
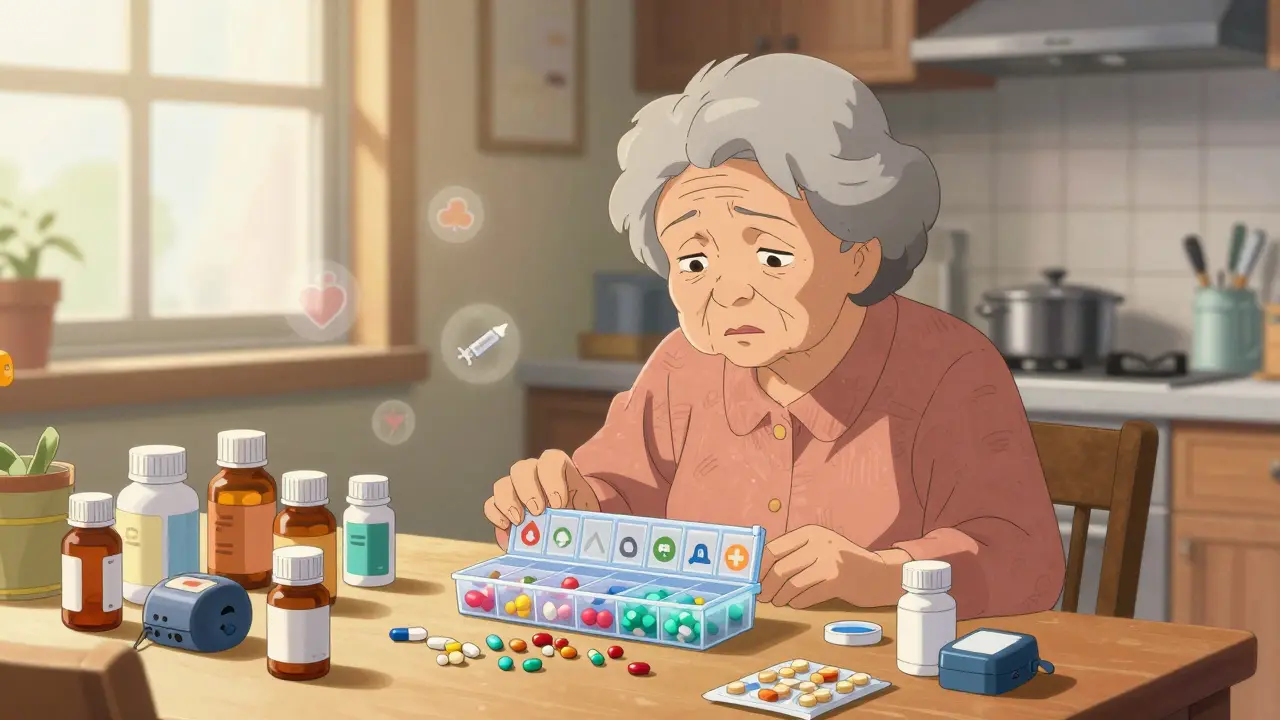
By the time someone reaches their 70s or 80s, it’s common to be taking five, ten, or even more medications every day. Some are for blood pressure, others for diabetes, arthritis, heart rhythm, sleep, or depression. Each one comes with its own schedule-morning, noon, night, with food, without food, on an empty stomach. Before long, the pill organizer looks like a science experiment gone wrong.
This isn’t just inconvenient. It’s dangerous. A 2020 study in the Journal of the American Geriatrics Society found that over half of older adults living at home struggle to keep track of their meds. Missed doses, double doses, mixing up pills-these aren’t mistakes. They’re symptoms of an overloaded system. And when people can’t manage their meds, hospital visits go up, independence goes down, and quality of life suffers.
The good news? Most of these regimens can be simplified-without losing effectiveness. The key isn’t cutting pills. It’s rearranging them smarter.
What Medication Simplification Actually Means
Simplifying a medication regimen doesn’t mean stopping drugs. It means making them easier to take-without changing what they do. Think of it like streamlining a morning routine: instead of brushing your teeth, flossing, rinsing, and using mouthwash at different times, you do it all in one step with a single product. Same goal. Less effort.
There are three main ways this happens:
- Combining pills: Switching from two separate pills (say, a blood pressure pill and a cholesterol pill) to one combination tablet.
- Reducing frequency: Switching from a pill taken three times a day to one taken just once.
- Using long-acting forms: Replacing short-acting insulin injections with a longer-lasting version that works for 24 hours.
A 2020 trial across 1,500 older adults in the U.S. found that 41% of medication schedules could be simplified just by adjusting when and how often pills were taken. In Australia, pharmacists using the MRS GRACE tool were able to simplify regimens for 58% to 60% of aged care residents.
And it works. When people take fewer pills at fewer times, they’re more likely to stick with them. One study showed that after simplification, self-reported adherence improved by nearly 30% in patients with heart disease.
The Five-Step Process for Simplifying Medications
Simplification isn’t a quick fix. It’s a careful, step-by-step process that requires time, teamwork, and a full picture of what the person is actually taking.
- Get the full list: Start with a best possible medication history. That means gathering every prescription, over-the-counter drug, vitamin, supplement, and herbal remedy-even the ones the person forgot to mention. Studies show that on average, there are six discrepancies between what doctors think a patient is taking and what they’re actually taking.
- Check what’s still needed: Not every pill is still necessary. Some were prescribed years ago and never reviewed. Others might be redundant. This step is called deprescribing. For example, if someone’s blood pressure is stable and they’re on two different BP meds, one might be safely removed.
- Look for combo options: Ask: Can two pills become one? For instance, many blood pressure and cholesterol medications now come in fixed-dose combinations. A single tablet can replace two separate pills.
- Switch to once-daily versions: Many drugs have extended-release forms. A diuretic taken twice a day? Maybe there’s a once-daily version. An antidepressant taken in the morning and evening? There may be a 24-hour capsule.
- Match timing to life: Can a pill be taken with breakfast instead of requiring an empty stomach? Can a nighttime dose be moved to morning if it’s not affecting sleep? The goal is to tie doses to daily routines-like meals, bedtime, or a nurse’s visit-not to rigid medical clocks.
The MRS GRACE tool, developed in Australia and validated in 2020, guides pharmacists through these steps with five simple questions. Training takes just two hours. But even without the tool, any provider can start by asking: “Can this be easier?”
When Simplification Works Best-and When It Doesn’t
Not all medications respond the same way. Some classes benefit hugely. Others need more caution.
Great candidates for simplification:
- Antihypertensives: Many blood pressure pills can be switched to once-daily versions. A 2020 review found improved adherence with simpler schedules.
- Antidepressants and antipsychotics: German studies showed fewer side effects and better compliance when dosing was reduced to once daily.
- Insulin: Long-acting insulins like glargine or degludec can replace multiple daily injections for many older adults.
- Statins: Most cholesterol meds are already once-daily. But if someone’s on two different statins, one can often be dropped.
Tricky cases:
- Thyroid meds: Levothyroxine must be taken on an empty stomach, usually 30-60 minutes before breakfast. You can’t just move it to lunch.
- Diabetes pills: Some, like metformin, cause stomach upset if taken without food. Others, like sulfonylureas, need to be timed with meals to avoid low blood sugar. Simplifying here can be risky without close monitoring.
- Anticoagulants: Warfarin requires regular blood tests. Even if dosing is simplified, monitoring can’t be.
One 2020 study in Australia found that while 83% of simplification efforts improved adherence, only about half led to measurable improvements in blood pressure, glucose, or cholesterol. That doesn’t mean it’s useless. It means adherence is the first step-and health outcomes follow, slowly.
Real-Life Impact: What Happens When Regimens Get Simple
In a nursing home in Perth, staff used the MRS GRACE tool to review 50 residents’ meds. They cut the average number of daily doses from 7.2 to 4.1. Medication errors dropped by 30%. Nurses reported less stress. Residents felt more in control.
One woman, 84, was taking 12 pills a day-some at 7 a.m., others at noon, 6 p.m., and 10 p.m. She often missed doses. After simplification: five pills, all taken with breakfast or dinner. She started taking them regularly. Her blood pressure improved. She told her daughter, “I finally feel like I’m not on a medicine schedule. I’m just living.”
Another case: a man with heart failure and diabetes was taking six pills at three different times. His daughter had to remind him every day. After switching to two combination pills taken twice daily-with clear labels and a weekly pillbox-he started taking them without help. His HbA1c dropped. He stopped falling.
These aren’t rare stories. They’re the norm when simplification is done right.
Barriers to Getting It Done
Despite the evidence, simplification still isn’t routine. Why?
- Time: A full medication review takes 30-60 minutes per person. Most doctors don’t have that kind of time in a 15-minute visit.
- Training: Only 35% of pharmacy schools in the U.S. teach medication simplification as part of geriatric training.
- System gaps: Electronic health records don’t always flag complex regimens. A 2022 update to Epic’s system now includes a complexity score-but most clinics haven’t turned it on.
- Prescribing habits: A 2020 survey found only 40% of primary care doctors routinely consider pill burden when prescribing to older adults.
And then there’s the fear: “What if we take something away and something bad happens?” But the bigger risk is doing nothing. The Journal of the American Medical Directors Association found that 56% of home care patients had regimens that could be simplified-and only half of those changes were ever made.
What Families and Caregivers Can Do
You don’t need to be a doctor to help. Here’s how:
- Make a list: Write down every pill, supplement, and cream. Include dose, time, and reason. Bring it to every appointment.
- Ask the pharmacist: Pharmacists are medication experts. Ask: “Can any of these be combined? Made once-daily? Stopped?”
- Use tools: Try a pill organizer with alarms. Use apps like Medisafe or MyTherapy to track doses.
- Speak up: If the person is confused, overwhelmed, or skipping doses, say so. Don’t assume it’s just aging.
- Push for a review: Request a “medication therapy management” session-many Medicare Advantage plans cover it for free.
One son in Seattle told us: “I thought my dad was just forgetful. Turns out, he had 11 pills a day. We cut it to four. He hasn’t missed one since.”
The Future of Medication Simplicity
More systems are catching on. Australia now requires aged care facilities to use some form of simplification. Germany pays pharmacists extra for doing medication reviews. The U.S. Medicare Advantage plans are starting to reward hospitals for reducing readmissions linked to poor medication management.
Future tools will likely include AI-driven alerts in EHRs that flag high-pill-count patients and suggest simplification options. The University of Sydney’s ongoing trial will show whether using MRS GRACE in nursing homes cuts errors and hospital stays long-term.
But the real breakthrough won’t come from tech. It’ll come from changing the mindset: Less isn’t worse. Simpler isn’t lazy. Easier isn’t dangerous-it’s essential.
Frequently Asked Questions
Can you really simplify medications without losing effectiveness?
Yes. Studies show that switching to combination pills or once-daily forms doesn’t reduce effectiveness-it often improves it. For example, a single pill combining a blood pressure and cholesterol drug works just as well as taking two separate pills. The key is matching the new schedule to how the drug works in the body. Pharmacists use evidence-based guidelines to ensure safety.
What if my loved one takes a pill at a specific time for a reason?
Some medications need specific timing-like thyroid pills on an empty stomach or statins at night. These aren’t always flexible. But many others are. A pharmacist can help sort which ones are critical and which can be moved. The goal isn’t to ignore medical logic-it’s to find where flexibility exists without risking safety.
Is it safe to stop a medication just to simplify?
Never stop a medication without consulting a doctor or pharmacist. But deprescribing-removing drugs that are no longer needed-is a safe and common part of simplification. For example, a 90-year-old on a blood thinner after a minor stroke five years ago might not need it anymore. A careful review can identify these cases safely.
How long does it take to see results after simplifying?
Adherence often improves within days or weeks-people start taking their pills because it’s easier. Clinical improvements, like lower blood pressure or better blood sugar, usually take weeks to months. The biggest win is fewer missed doses and less stress.
Who can help with medication simplification?
A geriatric pharmacist is the best person to lead this. Many hospitals and community pharmacies offer free medication reviews. Medicare Advantage plans often cover Medication Therapy Management (MTM) sessions. Ask your doctor for a referral. You can also call your local Area Agency on Aging-they often connect families with pharmacists who specialize in senior care.





rahulkumar maurya
February 4, 2026 AT 09:48Alec Stewart Stewart
February 4, 2026 AT 11:34Demetria Morris
February 6, 2026 AT 08:38Geri Rogers
February 8, 2026 AT 03:10Samuel Bradway
February 9, 2026 AT 07:33Alex LaVey
February 10, 2026 AT 16:31caroline hernandez
February 11, 2026 AT 21:18Jhoantan Moreira
February 13, 2026 AT 20:41Meenal Khurana
February 14, 2026 AT 23:12Joy Johnston
February 15, 2026 AT 02:56Alec Stewart Stewart
February 16, 2026 AT 06:06