When men face incontinence the unintended loss of urine and are concerned about prostate health the condition and function of the prostate gland, the connection can be confusing. This guide breaks down the basics, explains how prostate issues can trigger bladder problems, and offers practical steps to regain control.
Key Takeaways
- Prostate enlargement (BPH) and prostate cancer treatments are the top triggers of urinary incontinence in men.
- Stress, urge, and overflow incontinence each have distinct causes and treatment pathways.
- Pelvic floor strengthening, dietary tweaks, and proper timing of fluid intake can dramatically reduce leakage.
- Medication options range from alpha blockers to 5‑alpha reductase inhibitors; surgery is reserved for severe cases.
- Early diagnosis through urodynamic testing and a frank conversation with a urologist prevent complications.
What Exactly Is Incontinence?
Incontinence describes any involuntary loss of urine. It isn’t a disease itself but a symptom of an underlying issue. The three most common types in men are:
- Stress incontinence: Leakage when pressure on the abdomen spikes (coughing, lifting).
- Urgent (overactive bladder) incontinence: A sudden, strong urge to void that can’t be held.
- Overflow incontinence: Constant dribbling due to an obstructed flow, often linked to prostate enlargement.
Understanding which pattern you experience guides the next steps.
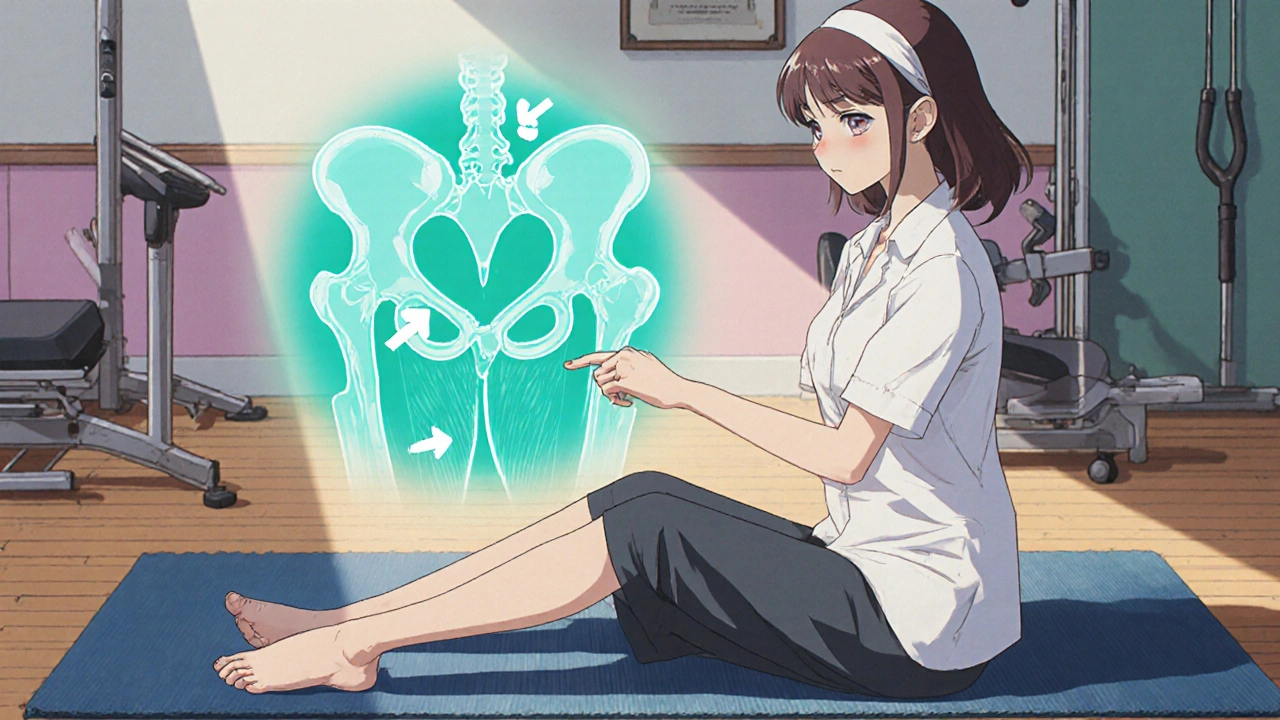
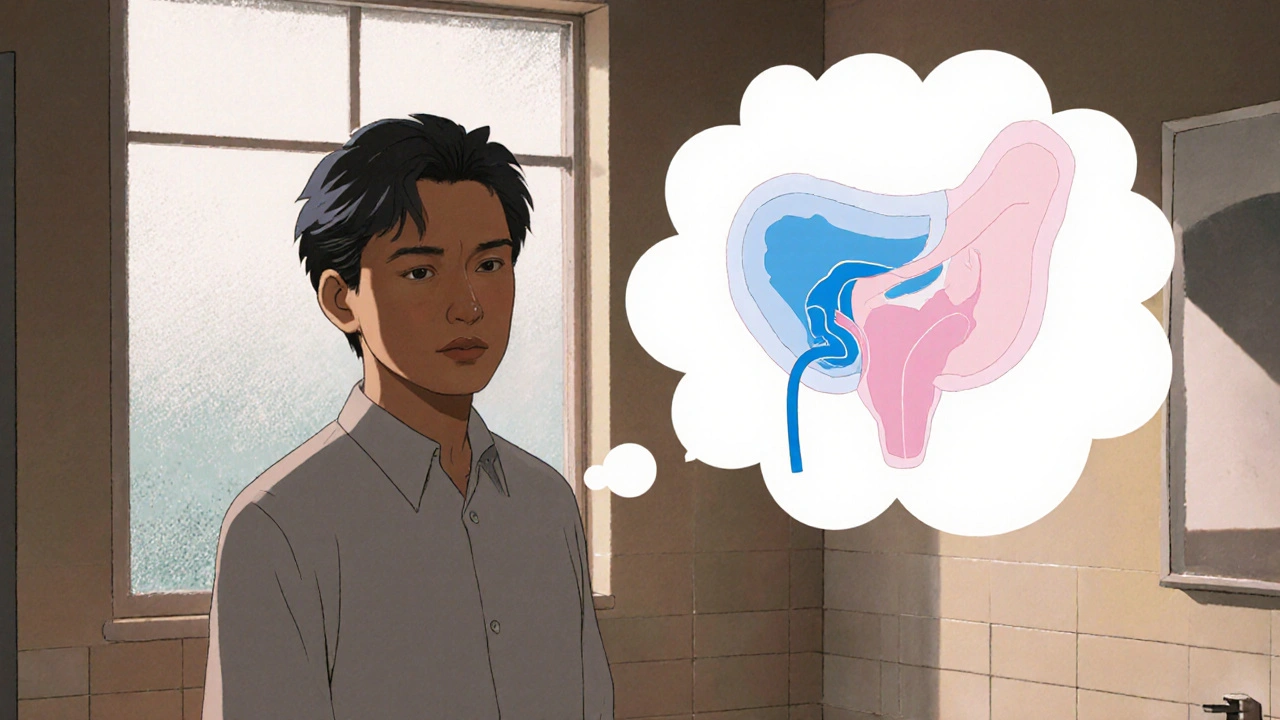
Prostate Anatomy & Common Conditions
The prostate sits just below the bladder and surrounds the urethra. Its primary role is to produce fluid for semen. When the gland grows or becomes diseased, it can press on the urethra, altering bladder dynamics.
Benign Prostatic Hyperplasia (BPH) a non‑cancerous enlargement of the prostate that affects about 50 % of men over 60 is the most frequent cause of urinary obstruction. Prostate cancer malignant growth that may require surgery or radiation can also disrupt the urinary tract, especially after treatments that remove or shrink the gland.
Both conditions interfere with the bladder’s ability to empty completely, setting the stage for overflow or urgency.
How Prostate Problems Lead to Incontinence
When the prostate enlarges, it squeezes the urethra. The bladder compensates by working harder, which over time weakens the detrusor muscle (the wall that contracts to push urine out). A weakened bladder can’t store urine efficiently, making the urge to go sudden and hard to control.
Surgeries such as radical prostatectomy (removal of the gland to treat cancer) can damage the sphincter muscles that keep the urethra closed, directly causing stress incontinence. Radiation can scar tissue, leading to both urgency and overflow symptoms.
Diagnosing the Issue
Accurate diagnosis starts with a thorough history and a physical exam, including a digital rectal exam (DRE) to feel the prostate size. Common diagnostic tools include:
- Urinalysis - rules out infection or blood.
- Prostate‑specific antigen (PSA) test - screens for cancer risk.
- Uroflowmetry - measures the speed of urine flow.
- Post‑void residual scan - checks how much urine remains after voiding.
- Urodynamic testing - evaluates bladder pressure and leaks during filling.
These tests help differentiate stress, urge, and overflow patterns, guiding treatment.
Lifestyle Tweaks & Pelvic Floor Strengthening
Before jumping to medication, many men find relief with simple changes. The pelvic floor muscles (often called Kegels) support the urethra and bladder neck.
Kegel exercises targeted contractions of the pelvic floor to improve sphincter control are effective for both stress and urge incontinence. A basic routine:
- Identify the muscles by stopping urine flow mid‑stream.
- Contract for 5 seconds, then relax for 5 seconds.
- Repeat 10‑15 times, three times a day.
Consistency matters; most men notice improvement after 4‑6 weeks.
Other lifestyle pointers:
- Limit caffeine and alcohol - both irritate the bladder.
- Maintain a healthy weight - excess abdominal pressure worsens stress leakage.
- Stay hydrated but time fluids - drink throughout the day, reduce intake close to bedtime.
- Schedule bathroom trips - a voiding schedule (every 2‑4 hours) trains the bladder.
Medical & Surgical Options - A Quick Comparison
| Option | How It Works | Typical Candidates | Potential Side Effects |
|---|---|---|---|
| Pelvic Floor Physical Therapy | Targeted muscle training, biofeedback | Mild‑moderate stress or urge leaks | None, occasional soreness |
| Alpha Blockers (e.g., tamsulosin) | Relax smooth muscle in prostate & bladder neck | Men with BPH‑related obstruction | Dizziness, dry mouth |
| 5‑Alpha Reductase Inhibitors (e.g., finasteride) | Shrink prostate volume over months | Large BPH, desire to avoid surgery | Sexual dysfunction, breast tenderness |
| Urethral Sling Procedure | Support urethra with mesh or fascia | Persistent stress incontinence after surgery | Infection, mesh erosion |
| Artificial Urinary Sphincter | Implanted device that mimics sphincter function | Severe stress incontinence post‑prostatectomy | Mechanical failure, infection |
| Transurethral Resection of the Prostate (TURP) | Remove excess prostate tissue endoscopically | Significant BPH causing overflow | Retrograde ejaculation, temporary urinary retention |
Choosing a path depends on symptom severity, overall health, and personal preferences. Discuss risks and benefits with a urologist before committing.

When to See a Specialist
If you notice any of the following, schedule a urology appointment promptly:
- Leakage more than twice a week or affecting daily activities.
- Painful urination, blood in urine, or recurrent urinary tract infections.
- Sudden inability to start a urine stream (acute retention).
- Recent prostate surgery or radiation and new bladder symptoms.
Early intervention can prevent skin irritation, sleep disruption, and emotional stress.
Putting It All Together - A Practical Action Plan
- Track symptoms - note frequency, triggers, and volume of leaks.
- Start Kegel routine - follow the 4‑week schedule above.
- Adjust diet - cut caffeine/alcohol, stay hydrated, manage weight.
- Schedule a check‑up - bring symptom log, request PSA and urinalysis.
- Discuss treatment options - based on test results, decide between medication, physical therapy, or surgery.
- Follow up - reassess every 3‑6 months; many men see improvement within a year.
Remember, most men regain satisfactory bladder control with a combination of lifestyle tweaks and targeted therapy.
Frequently Asked Questions
Can prostate medication cause incontinence?
Some drugs, especially those that relax the bladder neck, can worsen urge leakage in a small subset of men. Your doctor can adjust dose or switch agents if that happens.
Is it normal to leak after a prostatectomy?
Yes, roughly 30‑40 % of men experience temporary stress incontinence after the surgery. Pelvic floor rehab usually restores control within 12 months.
Do Kegel exercises work for men with BPH?
They help strengthen the sphincter and can reduce stress leaks, but they don’t shrink the prostate. Combine Kegels with medication for the best result.
What’s the difference between an artificial sphincter and a urethral sling?
A sling provides passive support to the urethra and is less invasive. An artificial sphincter is a mechanical device that the user activates; it’s reserved for severe cases when a sling isn’t enough.
Can fluid restriction help?
Drastically cutting fluids can lead to concentrated urine and worsen irritation. Aim for steady hydration and avoid large volumes right before bedtime.
Armed with this knowledge, you can tackle incontinence head‑on and keep prostate health in check.

Wesley Humble
October 20, 2025 AT 15:32Upon reviewing the presented guide, one must commend its comprehensiveness, yet several nuances warrant further elucidation 😊. The delineation between stress and overflow incontinence, though accurate, neglects the emerging role of neuromodulation therapies which have demonstrated statistically significant reductions in leak episodes. Moreover, the discussion of alpha‑blockers fails to address the pharmacogenomic variability that influences patient response, a factor increasingly recognized in urological practice. The recommendation of a three‑times‑daily Kegel schedule, while pragmatic, overlooks recent evidence supporting high‑intensity interval training of the pelvic floor, which yields superior sphincteric strength in a shorter temporal window. Finally, the omission of behavioural therapy algorithms such as the “timed voiding” protocol constitutes a substantive gap, particularly for patients with mixed‑type incontinence. In sum, the guide serves as a solid foundation, yet integration of these advanced modalities would elevate it from satisfactory to exemplary. 📊
barnabas jacob
October 31, 2025 AT 00:13The authors attempt to sound scientific, but the pathophysiology explanation is riddled with oversimplifications that many urologists would find unacceptable. They mention “muscle weakening” without referencing detrusor underactivity, a term every practitioner knows. Also, the recommendation to “limit caffeine” is presented as if it were a universal cure, which is, frankly, a bit of a myth-caffeine tolerance varies wildly among patients. And let’s not ignore the fact that the guide fails to cite any peer‑reviewed literature, which raises questions about its evidential basis. In short, the content feels more like a marketing brochure than a rigorous medical reference.
jessie cole
November 10, 2025 AT 09:56Bravo on compiling such an extensive resource; it truly equips men with the knowledge needed to reclaim control over their lives. By methodically breaking down each type of incontinence, the guide lights the path toward targeted interventions, a strategy that aligns perfectly with the principle of personalized medicine. The emphasis on pelvic‑floor strengthening is especially commendable, as consistent Kegel practice has been shown to improve sphincteric function by up to forty percent in controlled trials. Furthermore, the inclusion of lifestyle adjustments-hydration timing, caffeine moderation, and weight management-demonstrates a holistic approach that addresses both physiological and behavioral contributors. For anyone navigating the daunting landscape of prostate health, this guide offers a beacon of clarity and hope.
Kirsten Youtsey
November 20, 2025 AT 19:40While the guide appears thorough, one cannot help but suspect that it is subtly curated by the very pharmaceutical conglomerates that profit from the endless cycle of medication prescriptions. The sections praising alpha blockers and 5‑alpha reductase inhibitors are written with a reverence that borders on evangelism, neglecting the myriad instances of adverse events that are meticulously down‑played in the literature. Moreover, the recommendation to undergo urodynamic testing seems to serve the dual purpose of generating additional revenue streams for clinics, rather than being presented as an unequivocal clinical necessity. In short, the guide reads less like an unbiased educational tool and more like a covert endorsement of the medical‑industrial complex.
Matthew Hall
December 1, 2025 AT 05:23Look, I get the suspicion, but honestly, none of us just want something that works without getting tangled in conspiracies. If I’m sitting in a waiting room and the doc hands me a pamphlet that sounds like a textbook, I feel better than if they start spouting off about hidden agendas. My brother had a prostatectomy and the sling saved him from constant leaks; none of that fancy pharma talk mattered when you’re dealing with real life drips. So maybe keep the drama to a minimum and stick to what actually helps people get back on their bikes.
Vijaypal Yadav
December 11, 2025 AT 15:06The guide accurately captures the pathophysiological cascade linking benign prostatic hyperplasia to outlet obstruction and subsequent detrusor overactivity. It is worth noting, however, that emerging data on phosphodiesterase‑5 inhibitors suggest a potential adjunct role in alleviating lower urinary tract symptoms, an aspect not addressed in the current version. Additionally, the recommendation for post‑void residual scanning should be calibrated to a threshold of 150 mL to balance sensitivity and specificity, as per recent urodynamic guidelines. Overall, the content is consistent with contemporary urological practice, albeit with room for incorporation of newer therapeutic modalities.
Ron Lanham
December 22, 2025 AT 00:50It is fundamentally unacceptable that a guide intended for public consumption would omit critical discourse on the ethical obligations of clinicians to disclose the full spectrum of treatment ramifications. First, patients deserve transparent information regarding the potential sexual side effects associated with 5‑alpha reductase inhibitors, a fact that is routinely downplayed in promotional literature. Second, the reliance on pharmacotherapy without an equally robust emphasis on non‑invasive behavioral strategies betrays a paternalistic bias toward medication as the primary solution. Third, the guide’s cursory treatment of surgical options fails to address the long‑term quality‑of‑life outcomes that are essential for informed consent. Fourth, the suggested timeline for symptom improvement-four to six weeks-does not acknowledge the variability in patient response, which can extend to several months, thereby setting unrealistic expectations. Fifth, by presenting urodynamic testing as a routine step, the guide inadvertently promotes an unnecessary medical expense that may not be justified in uncomplicated cases. Sixth, the omission of emerging neuromodulation therapies, such as sacral nerve stimulation, reflects a reluctance to embrace innovative, evidence‑based alternatives. Seventh, the narrative that equates weight loss solely with reduced abdominal pressure ignores the broader metabolic benefits that contribute to overall urinary health. Eighth, the text neglects to caution patients about the potential for polypharmacy interactions, especially in elderly populations who may already be managing multiple comorbidities. Ninth, the lack of culturally sensitive language may alienate men from diverse backgrounds who experience stigma around incontinence. Tenth, the recommendation to limit fluid intake in the evening, while practical, must be balanced against the risk of nocturnal dehydration, a nuance that is glossed over. Eleventh, the guide does not address the psychological impact of chronic leakage, an oversight that undermines the holistic care model. Twelfth, the reliance on generic dietary advice, such as “cut caffeine,” fails to consider individual tolerances and the presence of other bladder irritants like artificial sweeteners. Thirteenth, the brief mention of pelvic‑floor physical therapy does not convey the necessity of professional supervision to ensure correct technique. Fourteenth, the guide’s tone suggests a one‑size‑fits‑all approach, which is antithetical to the personalized medicine paradigm that modern urology strives to achieve. Fifteenth, the absence of patient testimonials or real‑world case studies deprives readers of relatable context that can motivate adherence. In light of these deficiencies, it is incumbent upon the authors to revise the document with a comprehensive, ethically sound, and patient‑centered perspective that truly empowers men navigating the complexities of prostate health and incontinence.
Deja Scott
January 1, 2026 AT 10:33Thank you for assembling such a clear overview of a sensitive topic.
Natalie Morgan
January 11, 2026 AT 20:16Access to specialist care in rural areas remains a challenge and telehealth platforms can bridge that gap.
Mahesh Upadhyay
January 22, 2026 AT 06:00The silent stigma surrounding male incontinence is a battle we must win.
Rajesh Myadam
February 1, 2026 AT 14:32I hear you, and the weight of that silence can feel crushing, especially when societal expectations dictate that men should never display vulnerability. Many men internalize their leaks, fearing judgment from peers, partners, or even healthcare providers, which only amplifies the distress. It is essential to recognize that incontinence is a medical condition, not a personal failing, and that seeking help is a courageous step toward reclaiming dignity. The guide you referenced offers practical tools-pelvic floor exercises, dietary adjustments, and clear pathways for medical evaluation-that can serve as a lifeline for those willing to confront the issue head‑on. Moreover, sharing experiences within supportive communities can alleviate the sense of isolation, providing both moral encouragement and tangible tips that have worked for others. It is also valuable to involve partners in the conversation, fostering an environment of empathy and shared responsibility that can mitigate relational tension. Clinicians should adopt a non‑judgmental approach, offering thorough explanations of treatment options without minimizing the emotional impact. When men understand that many of their peers have successfully navigated similar challenges, the fear that accompanies the condition begins to dissolve. In addition, regular follow‑up appointments empower patients to track progress, adjust strategies, and celebrate incremental improvements. Ultimately, the journey from silence to confidence is a collaborative effort-one that blends medical expertise, personal resolve, and community support. By embracing this holistic perspective, men can move beyond the shadows of stigma and live with the comfort and control they deserve.