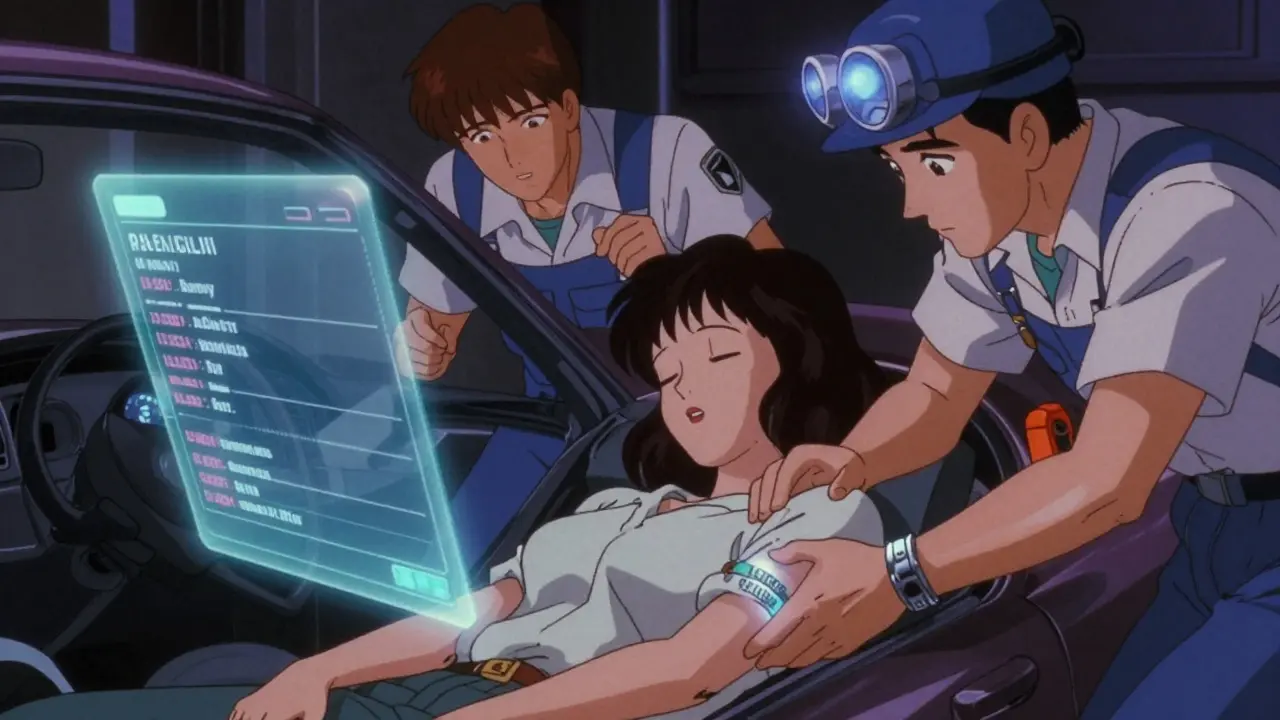
Every year, thousands of people end up in emergency rooms with life-threatening medication errors - not because doctors made a mistake, but because no one knew what drugs they were taking. In those first critical minutes, when a patient is unconscious, confused, or unable to speak, a simple metal band on the wrist can be the difference between life and death. Medical alert bracelets aren’t just jewelry. They’re emergency lifelines, especially when it comes to drug safety.
Why Your Medications Could Kill You in an Emergency
Imagine you’re in a car crash. You’re knocked out. The paramedics arrive. They see you’re bleeding, your vitals are dropping, and they need to act fast. They reach for the nearest IV bag - maybe morphine for pain, maybe antibiotics for infection. But what if you’re allergic to penicillin? What if you’re on warfarin and that IV fluid could trigger internal bleeding? Without knowing your meds, they’re guessing. And guessing in emergencies can be deadly. A 2022 study in the Journal of Emergency Medicine found that 37% of ER errors involve medications. That’s not rare. That’s routine. And half of those errors happen because the patient couldn’t tell the team what they were taking. That’s where medical alert bracelets come in. They don’t replace communication - they make it possible when communication is gone.What Information Actually Saves Lives
Not all medical IDs are created equal. A bracelet that says “Diabetic” doesn’t help if you’re in a hypoglycemic crisis and need glucose - not insulin. A bracelet that says “Allergic to Penicillin” is good. But if it says “Allergic to Antibiotics,” that’s too vague. First responders need specifics. According to the American College of Emergency Physicians (ACEP), the top three things to list on your bracelet are:- Drug allergies - especially penicillin (affects 1 in 10 Americans), latex, NSAIDs like aspirin, and sedatives.
- Critical medications - blood thinners like warfarin, rivaroxaban, or apixaban. These change how you’re treated in trauma. Giving you a clot-busting drug when you’re already on a blood thinner? That’s a recipe for internal bleeding.
- Chronic conditions requiring special protocols - Type 1 vs. Type 2 diabetes, heart failure, epilepsy, or kidney disease. Each changes how emergency teams handle fluids, meds, and monitoring.
Traditional vs. QR Code Bracelets: Which One Works Better?
You’ve probably seen the classic stainless steel bracelet with tiny engraved letters. It’s durable. It’s timeless. But it’s also limited. Most can fit only 3 to 5 pieces of critical info. That’s not enough if you’re on five different medications, have three allergies, and have a pacemaker. Enter QR code bracelets. Launched by MedicAlert Foundation in 2018, these look like regular bracelets - but when scanned with a smartphone, they open a full digital profile. That profile can include:- Full medication list with dosages
- Prescribing doctors’ contact info
- Recent lab results
- Emergency contacts
- NDC drug codes (new as of March 2024) so pharmacists can identify exact drugs even if brand names differ
Real Stories: How a Bracelet Prevented a Death
On Reddit, user ‘AllergicAmy’ shared her story from 2022. She went to the ER for appendicitis. The doctor ordered penicillin - a standard antibiotic. Her bracelet said: “ANAPHYLACTIC TO PENICILLIN.” The nurse paused. Double-checked. Cancelled the order. Later, the nurse told her: “We were about to give it to you. You’d have been dead in minutes.” That’s not an outlier. Medical Guardian’s 2023 study tracked 142 cases where medical ID bracelets directly prevented fatal drug interactions. Most involved blood thinners and emergency anticoagulants. In one case, a man with atrial fibrillation was brought in after a fall. His bracelet listed apixaban. The ER team skipped the usual clot-prevention protocol - because they knew he was already on a blood thinner. He walked out two days later. Trustpilot reviews for MedicAlert show 4.7 out of 5 stars. Sixty-three percent of users say they bought it for drug safety. One man with Type 1 diabetes wrote: “I had a low blood sugar episode at the gym. The EMTs saw my bracelet, gave me glucose, and saved me. I didn’t have to explain anything.”The Hidden Problem: Outdated Information
Here’s the ugly truth: 35% of people never update their medical ID after a medication change. That’s according to the American Pharmacists Association. You switch from warfarin to rivaroxaban? You get a new prescription for insulin? You forget to change your bracelet. Now you’re carrying dangerous misinformation. A 2023 JAMA Internal Medicine study audited 500 emergency cases. Nineteen percent of bracelets had outdated or incomplete info. That’s almost 1 in 5. And in an emergency, bad info is worse than no info. It leads to wrong decisions. The fix? Use a digital profile with auto-updates - like MedicAlert’s SmartProfile. Or set a calendar reminder every time your meds change. If you’re on a new drug, write it down. Then update your bracelet within 48 hours. Don’t wait. Don’t assume you’ll remember.Who Needs One the Most?
You don’t have to be elderly or chronically ill to need a medical alert bracelet. But some groups benefit more:- People on blood thinners - 41% of them wear one, per the 2024 National Health Interview Survey.
- Those with severe allergies - 33% wear one, especially if they’ve had anaphylaxis.
- Diabetics - 28% wear one, especially if they use insulin.
- People on multiple medications (five or more) - risk of interaction skyrockets.
- Anyone with cognitive issues - dementia, autism, or brain injury - who might not communicate clearly.

Cost, Quality, and What to Buy
You don’t need to spend hundreds. Basic engraved metal bracelets start at $49.99 from MedicAlert Foundation. QR code versions start at $69.99, plus $59.99/year for the digital profile. Medical Guardian’s 2025 system - which includes a wearable alarm that calls for help - starts at $29.95/month. That’s a full safety net: the bracelet tells medics what to do; the alarm gets them there faster. Customer service matters. MedicAlert scored 4.3/5 in J.D. Power’s 2024 study. Smaller brands? Average 3.1/5. You want a company that answers the phone. You want guides on how to write your info clearly. You want updates that actually work.What Hospitals Are Doing Now
The game is changing. Since the 2022 CARES Act, U.S. hospitals are required to check for medical IDs during emergency intake. 67% now have formal protocols. Epic and Cerner - the two biggest hospital software systems - are building direct links to digital medical ID profiles. Soon, when you’re admitted, your bracelet’s QR code might pull up your full EHR. No more manual entry. No more guesswork. The FDA’s 2023 Medical ID Modernization Initiative is pushing for standard formats. That means no more cryptic abbreviations. No more “BS” for “blood thinner.” Just clear, consistent language anyone can read.Final Thought: It’s Not About Fear. It’s About Control.
A medical alert bracelet isn’t a sign you’re sick. It’s a sign you’re smart. You’re taking control of your safety. You’re saying: “If I can’t speak, let my body speak for me.” It’s not about living in fear of emergencies. It’s about making sure, when one happens, you’re not a mystery to the people trying to save you. Your meds matter. Your allergies matter. Your life matters. Wear it every day. Update it every change. And if you’re unsure what to put on it - call your pharmacist. Ask them to help you write it. They’ve seen the mistakes. They know what saves lives.Do medical alert bracelets really work in emergencies?
Yes. First responders are trained to check wrists and necks for medical IDs. In 89% of cases where a bracelet is present, responders use the information correctly, according to GoodRx. A 2022 study from the American College of Emergency Physicians found medical ID bracelets reduce medication errors by 28% in unconscious patients.
What should I write on my medical alert bracelet?
Prioritize: 1) Drug allergies (e.g., "ALLERGIC TO PENICILLIN"), 2) Critical medications (e.g., "ON WARFARIN" or "ON RIVAROXABAN"), 3) Chronic conditions needing emergency protocols (e.g., "TYPE 1 DIABETIC, INSULIN DEPENDENT"). Avoid vague terms like "allergic to antibiotics" - be specific. If space is limited, use abbreviations like "BP" for blood pressure meds, but only if they’re universally understood.
Are QR code bracelets better than engraved ones?
For most people, yes - especially if you take multiple medications or have complex health needs. Engraved bracelets are limited to 3-5 items. QR code versions link to a full digital profile with your complete meds, dosages, doctors, and allergies. They also auto-update with pharmacy data (like MedicAlert’s SmartProfile). The downside: they require a yearly fee and a smartphone to scan. But in an emergency, the extra detail saves lives.
How often should I update my medical alert bracelet?
Immediately after any medication change. If your doctor prescribes a new drug, stops one, or changes your dose, update your bracelet within 48 hours. The American Pharmacists Association says 35% of users never update theirs - creating dangerous misinformation. Use calendar reminders or digital profiles that auto-sync with your pharmacy to stay current.
Can I wear a medical alert bracelet if I’m young and healthy?
Absolutely. You don’t have to be elderly or chronically ill to need one. If you take any prescription medication - especially blood thinners, antidepressants, seizure meds, or insulin - you’re at risk of an unexpected emergency. Accidents happen. If you’re unconscious, no one will know what you’re taking. A bracelet ensures you’re not a mystery to first responders.






Alex Flores Gomez
January 29, 2026 AT 04:42Look, if you’re not wearing a medical ID, you’re basically telling EMTs to play Russian roulette with your meds. I’ve seen dudes with 12 prescriptions and no bracelet-then they get in a fender bender and the ER gives them morphine and warfarin together. Boom. Internal bleeding. Not dramatic. Not Hollywood. Just stupid. Wear the damn band.
Kacey Yates
January 29, 2026 AT 22:55QR codes are the future but dont forget the basics. My grandma had a cheap engraved one that said 'ALLERGIC TO PENICILLIN' and it saved her life when she collapsed at the grocery store. No phone needed. No subscription. Just metal and clarity. Dont overcomplicate it.
Laura Arnal
January 31, 2026 AT 11:20Yessss this is so important!! 💪 I got mine after my cousin had a bad reaction and almost didn't make it. Now I wear mine every day-even to the gym. My pharmacist helped me write it and it took 5 minutes. Life-changing. You're not weak for wearing it-you're smart. ❤️
Robin Keith
January 31, 2026 AT 22:15It’s not merely about the bracelet-it’s about the metaphysical rupture between autonomy and vulnerability in the modern medical-industrial complex. We are reduced to data points, yet our bodies retain agency only when encoded in stainless steel or QR-activated cloud profiles. The irony is palpable: we outsource our very identity to corporate subscription models while pretending we’re in control. The bracelet is not a tool-it’s a symptom. A silent scream against the dehumanization of emergency care. And yet… I wear mine. Because even philosophy can’t stop a hemorrhage.
Kristie Horst
February 2, 2026 AT 15:12It’s admirable that you’re advocating for safety-but let’s be honest, most people won’t update their bracelets. The real issue isn’t technology. It’s human inertia. You can have the most advanced digital profile in the world, but if the user forgets to log in for six months, it’s just a fancy paperweight. And yes, I’m speaking from experience. I had a friend who switched from Eliquis to Xarelto and didn’t update her bracelet for nine months. She almost died. Don’t let your safety depend on your forgetfulness.
Andy Steenberge
February 3, 2026 AT 13:08My dad’s on five meds and has a pacemaker. He got the QR bracelet after his last ER visit. The nurse scanned it, pulled up his full history, and said, 'Holy crap, you’re on apixaban AND amiodarone-why didn’t you tell us?' He hadn’t even remembered. The bracelet saved us from a dangerous interaction. Honestly? Worth every penny. And yes, I remind him to check his profile every time he gets a new script. It’s not a chore-it’s care.
Laia Freeman
February 4, 2026 AT 17:10OMG I JUST GOT MINE!! 😍 I was so scared to wear it cause I thought it looked 'medical' and I'm only 27 but then I got a cute one with a little leaf design and now I'm obsessed. My doc said I'm on a blood thinner now after that weird clot thing and I was like 'wait, what if I get hit by a bus??' So I did it. Best decision ever. Also, my pharmacist wrote it for me-so easy. Everyone should do this. Like, seriously.
paul walker
February 5, 2026 AT 03:38My sister’s a nurse. She says 8 out of 10 unconscious patients don’t have IDs. And when they do, half the info’s wrong. I got mine last month. Simple. Stainless. 'ALLERGIC TO NSAIDS | ON WARFARIN'. No fluff. No subscription. Just facts. If you’re on meds, do this. It’s not optional.
Megan Brooks
February 6, 2026 AT 02:35While the technological advancements in digital medical IDs are commendable, one must not overlook the enduring efficacy of simplicity. The engraved bracelet, though limited in capacity, remains universally accessible, requiring no power source, no connectivity, and no corporate infrastructure. Its permanence is not a flaw-it is its strength. We must not confuse innovation with necessity. Clarity, not complexity, saves lives.
Ryan Pagan
February 7, 2026 AT 10:32Let’s cut the crap-QR bracelets are the real MVP. I’m on apixaban, metformin, lisinopril, and sertraline. No way in hell my wrist can fit all that in tiny letters. My QR bracelet auto-updates with my pharmacy. Last week, my doc switched me to a new blood thinner and boom-my bracelet changed overnight. No forgetting. No panic. No 'oh shit I forgot to update it.' That’s not tech-that’s peace of mind. And yeah, I pay the $60. Worth every cent.
Paul Adler
February 8, 2026 AT 12:33Interesting read. I’ve always thought of medical IDs as something for older folks or those with severe conditions. But the data here shows even young, seemingly healthy people on prescriptions are at risk. I never thought about it until my cousin had a seizure and they didn’t know she was on lamotrigine. The bracelet didn’t save her-but it would’ve helped. I’m getting one now. No more assumptions.