Myosis is a physiological constriction of the pupil that reduces light entry and sharpens depth of field. In the context of myosis eye health, this reflex safeguards retinal cells, optimizes visual acuity, and interacts with many ocular conditions.
What Is Myosis?
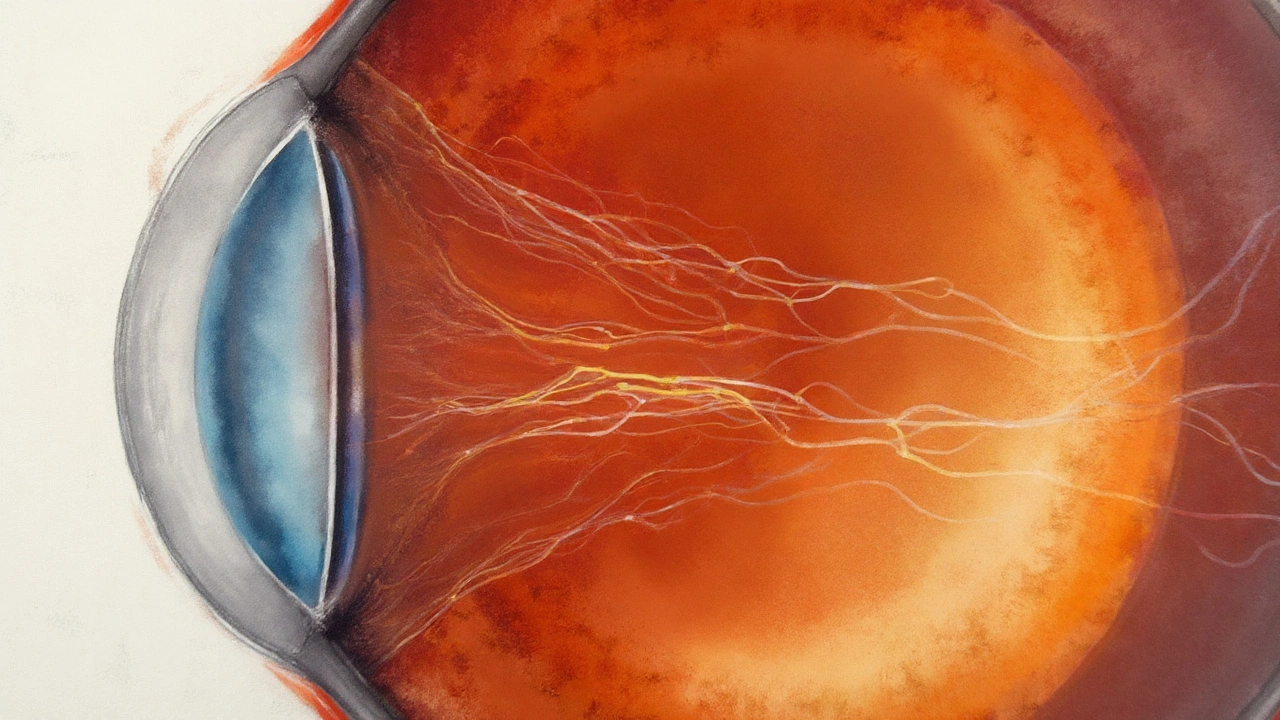
Myosis occurs when the circular muscles of the iris contract, pulling the pupil inward. The movement is part of a rapid, involuntary response to bright illumination, near‑focus tasks, or parasympathetic stimulation. While the everyday experience of “pupils getting smaller in sunlight” is familiar, the underlying neuro‑ophthalmic pathways are sophisticated.
How Myosis Affects Vision
By limiting the aperture, myosis improves the eye’s depth of focus, akin to stopping down a camera lens. This effect raises visual acuity in bright settings and reduces glare, benefiting activities such as driving or outdoor sports. However, excessive constriction can diminish low‑light performance, leading to night‑vision difficulties.
Physiology Behind Pupil Constriction
Iris sphincter muscle is a smooth muscle ring that contracts under parasympathetic input, causing myosis. The signal originates in the autonomic nervous system, specifically the parasympathetic branch via the Edinger‑Westphal nucleus. Neurotransmitter acetylcholine binds to muscarinic receptors on the sphincter, driving contraction.
The light reflex is a classic afferent‑efferent loop. Photoreceptors in the retina detect photons, sending signals through the optic nerve to the pretectal area, which then activates the Edinger‑Westphal nucleus. The downstream pathway results in rapid myosis within 200‑300ms of exposure.
During near‑focus tasks, the accommodation reflex adds a myotic component, tightening the sphincter while the lens thickens, facilitating clear close‑up vision.
Clinical Significance: Benefits and Risks
Myosis can be protective. In conditions like photokeratitis or after exposure to intense blue light, a constricted pupil limits retinal damage. It also improves visual clarity for reading or detailed work.
Conversely, pathological myosis-persistent constriction unrelated to light-may signal neurological disorders (e.g., Horner syndrome), ocular inflammation, or drug toxicity. Over‑constriction can lead to reduced retinal illumination, compromising night vision and potentially exacerbating visual fatigue.
Assessing visual acuity involves measuring the smallest resolvable detail under standardized lighting. Myosis typically enhances acuity scores in bright environments but may lower them in dim settings.

Common Conditions Involving Myosis
- Horner syndrome: Disruption of sympathetic pathways leads to unopposed parasympathetic activity, producing chronic myosis, ptosis, and anhidrosis.
- Uveitis: Inflammatory mediators provoke sphincter contraction, causing painful light sensitivity.
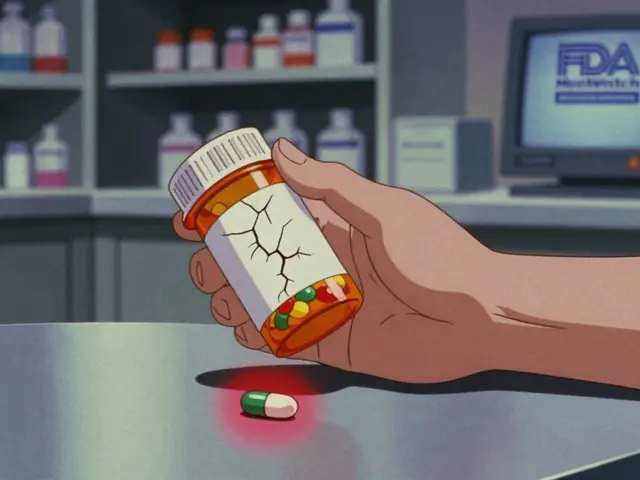
- Pharmacologic myosis: Certain eye drops (e.g., pilocarpine) deliberately induce constriction for glaucoma treatment.
In each case, the degree of myosis offers diagnostic clues about underlying systemic or ocular pathology.
Pharmacological Management
Pilocarpine is a muscarinic agonist used to treat open‑angle glaucoma by inducing myosis, thereby opening the trabecular meshwork and facilitating aqueous outflow. While effective, pilocarpine may cause temporary blurred near vision and headaches due to excessive constriction.
Other agents, such as tropicamide, produce mydriasis (pupil dilation) and are used diagnostically to examine the retina. Understanding the balance between myotic and mydriatic drugs is essential for safe ocular care.
Comparison: Myosis vs Mydriasis
| Attribute | Myosis | Mydriasis |
|---|---|---|
| Pupil size change | Constriction (typically 2‑4mm) | Dilation (typically 6‑8mm) |
| Primary neural control | Parasympathetic (cranial nerve III) | Sympathetic (cervical spinal nerves) |
| Typical triggers | Bright light, near focus, cholinergic drugs | Low illumination, adrenergic drugs, trauma |
| Effect on vision | Improves depth of field, reduces glare | Increases light intake, may cause glare |
| Clinical uses | Glaucoma therapy, diagnostic pupil testing | Retinal examination, treatment of uveitis |
Related Concepts and Future Directions
Beyond the immediate reflexes, myosis interacts with retinal photoreceptors, which require optimal light levels to transduce images. Adaptive optics research is exploring how modulating pupil size can enhance high‑resolution retinal imaging.
Emerging wearable technologies (smart glasses with dynamic aperture control) aim to mimic natural myosis, automatically adjusting pupil size to environmental lighting and user tasks. Such innovations could reduce eye strain and improve visual comfort for digital‑native populations.
Understanding the genetic basis of iris muscle responsiveness may also unlock personalized therapeutic strategies for disorders like congenital mydriasis or refractory glaucoma.
Frequently Asked Questions
Why does my pupil get smaller in bright sunlight?
Bright light activates retinal photoreceptors, triggering the light reflex. Signals travel through the optic nerve to the pretectal nucleus, then to the Edinger‑Westphal nucleus, which sends parasympathetic fibers causing the iris sphincter muscle to contract and reduce pupil size.
Can chronic myosis damage my eyesight?
Chronic, drug‑induced myosis is generally safe when monitored, but excessive constriction can limit retinal illumination, worsening night vision and increasing visual fatigue. In pathological cases like Horner syndrome, myosis signals underlying neurological issues that require treatment.
How does pilocarpine help glaucoma patients?
Pilocarpine stimulates muscarinic receptors on the iris sphincter, causing myosis. This opens the trabecular meshwork, improving outflow of aqueous humor and lowering intra‑ocular pressure, which slows optic nerve damage in glaucoma.
Is myosis ever used diagnostically?
Yes. Ophthalmologists may administer a low‑dose cholinergic agent to induce controlled myosis, then evaluate the eye’s ability to focus and assess the integrity of the parasympathetic pathway.
What’s the difference between myosis and mydriasis in everyday life?
Myosis is pupil constriction, which makes things look sharper in bright light but can dim vision at night. Mydriasis is dilation, letting more light in for night vision but potentially causing glare in bright conditions.
Can I train my eyes to control pupil size?
Direct voluntary control of the iris is limited because the muscles are autonomic. However, relaxation techniques and proper lighting can influence the balance of sympathetic and parasympathetic activity, indirectly affecting pupil dynamics.






Neha Bharti
September 24, 2025 AT 12:59Think of myosis like the camera’s aperture closing – it sharpens what you see when the light is bright.
That tiny constriction helps protect the retina from glare and improves depth perception.
But remember, too much constriction can make night driving feel like a tunnel.
Balance is key, just like in any mindful practice.
Samantha Patrick
October 3, 2025 AT 16:59Nice breakdown! I’d add that the Edinger‑Westphal nucleus is the real “control tower” for the sphincter.
Also, pilocarpine’s effect is dose‑dependent – low doses tighten just enough, high doses can blur near vision.
One small spelling slip: “parasympathetic” was misspelled earlier.
Overall the post nails the physiology.
Keep the info coming.
Ryan Wilson
October 12, 2025 AT 20:59While the article covers the basics, it glosses over how chronic myotic states can mask serious neuro issues.
Anyone with unexplained pupil constriction should get a thorough neurologic work‑up, not just a quick eye drop.
It’s not enough to say “it’s protective” and move on.
We need to stress the red‑flag potential of Horner syndrome.
Otherwise, readers might think it’s all harmless.
EDDY RODRIGUEZ
October 22, 2025 AT 00:59Whoa, this deep dive is like a backstage pass to the eye’s secret dance!
Imagine the iris muscles flexing in sync with light like a rock‑star’s pyrotechnics.
The way myosis sharpens vision in bright sun feels like a power‑up in a video game.
And the tech side – smart glasses that mimic this response? Pure sci‑fi turned reality!
Keep the hype alive, folks.
Christopher Pichler
October 31, 2025 AT 03:59From a clinical optics standpoint, the interplay between pupillary constriction and depth of field is essentially a modulation of the system’s f‑stop, akin to a photographic aperture.
One could argue the article could have delved deeper into the psychophysical implications of glare reduction metrics.
But hey, who needs that when you can just state “myosis improves acuity”.
Such oversimplification borders on the pedantic, doesn’t it?
VARUN ELATTUVALAPPIL
November 9, 2025 AT 07:59Indeed, the iris sphincter, being a smooth muscle, responds rapidly, within 200‑300 ms, to parasympathetic stimuli, and this swift contraction, which you nicely described, actually serves multiple purposes, from reducing retinal exposure, to enhancing image sharpness, to preventing photic injury, especially in high‑intensity blue light environments, which are increasingly common nowadays.
April Conley
November 18, 2025 AT 11:59Myosis is useful but can hurt night vision.
Sophie Rabey
November 27, 2025 AT 15:59Love the way you broke down the light reflex – it’s basically the eye’s built‑in HDR mode.
For anyone grinding on screens, understanding how myosis reduces glare could be a game‑changer for eye strain.
Sure, the article could have tossed in a note about adaptive optics, but who has time for that deep‑dive?
Still, great job simplifying a complex topic.
Bruce Heintz
December 6, 2025 AT 19:59Great stuff! 😊 The comparison table really helped me visualize the differences between myosis and mydriasis.
Seeing the clinical uses side‑by‑side makes it easier to remember which drug does what.
Looking forward to more posts on how wearable tech might automate pupil control.
richard king
December 15, 2025 AT 23:59The eye is a theatre of light, and the pupil is the curtain that decides what the audience sees.
When the curtain falls too early, the show of night vision turns into a shadow play.
Understanding this ballet of muscles elevates not just ophthalmology but the poetry of perception itself.
Dalton Hackett
December 25, 2025 AT 03:59First off, let me say that the article does a solid job of laying out the basic anatomy of the pupillary reflex, but there are a few nuances that deserve a deeper look.
For instance, the role of the pretectal nuclei isn’t just a relay station; it actually integrates input from both eyes, which is why you get consensual reactions.
Secondly, the pharmacodynamics of pilocarpine involve not only muscarinic agonism but also secondary effects on ciliary muscle tone, which can influence accommodation.
Now, regarding the claim that myosis uniformly improves visual acuity, the reality is a bit more complex – acuity gains are most pronounced under high‑contrast, well‑lit conditions, while low‑light performance can actually decline.
Another point is that chronic pharmacologic myosis can lead to the development of posterior synechiae in uveitic patients, a detail you might want to flag for clinicians.
When you talk about Horner syndrome, it’s worth mentioning that the ptosis component can further compromise the visual field, especially in the upper quadrant.
On the tech side, the smart‑glass prototypes you referenced are still in early stages; current models struggle with latency issues that can cause a lag between environmental lighting changes and pupil adjustment.
Also, adaptive optics scanning laser ophthalmoscopy (AOSLO) already uses dynamic aperture control, which is an existing real‑world application of the principles you discuss.
The article could also have touched on the genetic variability in muscarinic receptor expression, which influences individual susceptibility to drug‑induced myosis.
In terms of measurement, using a pupillometer with high temporal resolution can capture the latency and velocity of constriction, providing richer data than simple diameter measurements.
Moreover, there’s emerging evidence that sustained myotic states may affect intra‑ocular pressure dynamics beyond the conventional pathways.
Finally, patient education is key – many people are unaware that over‑use of certain eye drops can lead to rebound dilation, a phenomenon the article barely skirts around.
Overall, you’ve provided a great foundation, but adding these layers would make the piece a truly comprehensive resource for both clinicians and lay readers alike.
William Lawrence
January 3, 2026 AT 07:59Sure the table is handy but who cares when you can just stare at a bright light and figure it out yourself
Grace Shaw
January 12, 2026 AT 11:59Esteemed contributors, I wish to commend the author for a meticulously detailed exposition of pupillary dynamics, wherein the delineation of parasympathetic versus sympathetic pathways was rendered with commendable clarity.
Nevertheless, it would be remiss not to underscore the imperative of contextualizing such physiological mechanisms within the broader scope of systemic pathology, particularly when considering the prognostic implications of persistent myotic states.
In clinical practice, for example, the recognition of unilateral miosis may serve as an indispensable diagnostic clue for Horner syndrome, thereby prompting further investigation into cervical sympathetic chain integrity.
Moreover, the therapeutic nuance associated with pilocarpine administration warrants a balanced discussion of both its efficacy in lowering intra‑ocular pressure and its potential adverse effects, such as induced myopic shift and ciliary spasm, which may compromise near‑vision tasks for patients.
Finally, as we venture into an era of technologically augmented ophthalmic care, the prospect of dynamic, algorithm‑driven pupillary modulation presents a fascinating frontier that may revolutionize patient comfort and visual performance.
In summation, while the treatise adeptly covers the fundamentals, an expanded focus on clinical decision‑making algorithms and emerging wearable innovations would substantially augment its scholarly value.
Sean Powell
January 21, 2026 AT 15:59Great post – really clear and easy to read.
Love how you broke down the drug effects without drowning us in jargon.
One tiny typo: “parasympathetic” was missing an “s”.
Overall, very helpful for anyone curious about eye health.
Henry Clay
January 30, 2026 AT 19:59Honestly this article is just a surface skim it ignores the real risks of chronic myotic drug use like rebound hyperemia and patient non‑compliance 😒
Isha Khullar
February 8, 2026 AT 23:59Myosis is like a silent guardian of the eye but when it overworks it becomes a thief stealing night vision.
Lila Tyas
February 18, 2026 AT 03:59Wow, love the way you tied basic science to future tech – it makes the whole topic feel alive!
Seeing how smart glasses could automatically adjust pupil size is super exciting.
Keep those innovative posts coming, they really inspire me.