High drug costs can make life difficult for people with chronic conditions. If you're taking a brand-name medication, especially a specialty drug, your out-of-pocket costs might be overwhelming. Manufacturer Copay Assistance Cards are financial assistance tools offered by pharmaceutical companies to help cover part or all of your copay or coinsurance for specific medications. These cards are designed for people with private insurance, but they don't work for Medicare Part D or Medicaid recipients due to federal rules. Let's walk through exactly how to use them and what you need to watch out for.
How to get and use a copay assistance card
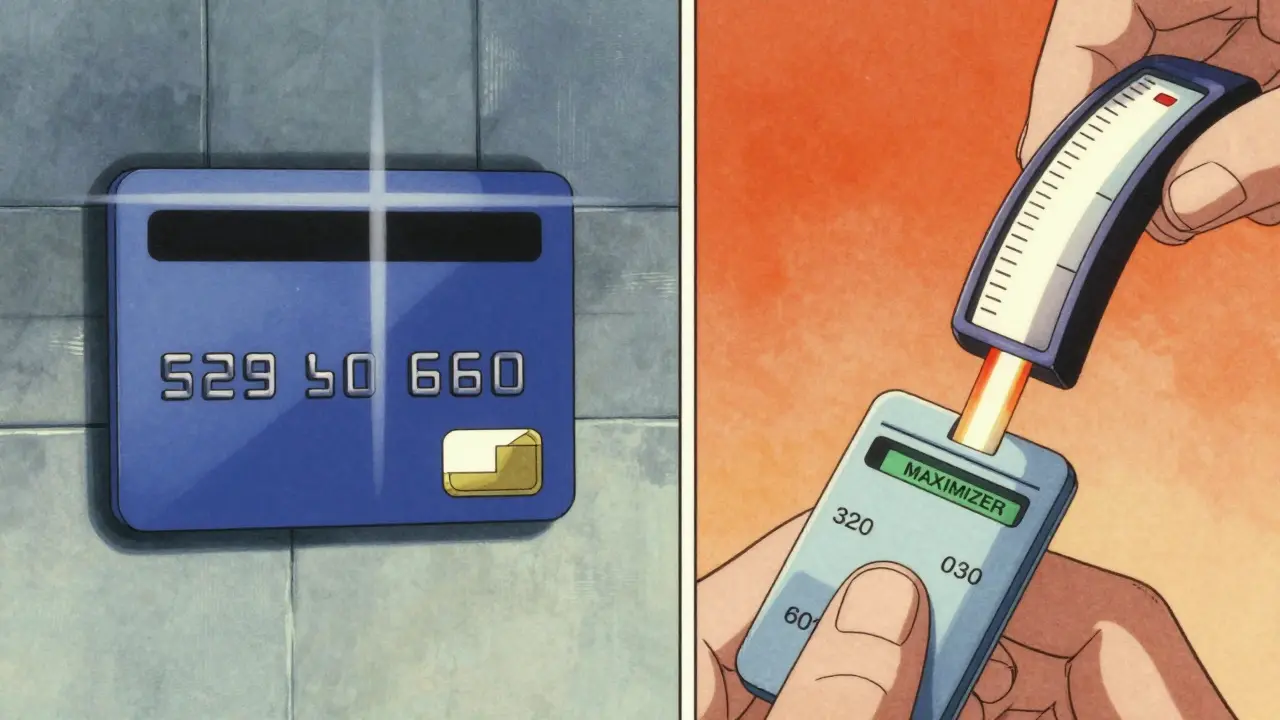
Getting a copay assistance card is simple. First, visit the manufacturer's website for your specific medication. Look for a "Patient Assistance" or "Copay Card" section. You'll need to enter basic info like your name, insurance details, and prescription information. The site will check if you qualify. If you do, you can download the card immediately or get a digital version sent to your phone. When filling your prescription, hand the card to the pharmacist along with your insurance. The pharmacy will process it automatically, and the manufacturer will cover part or all of your copay. For example, if your medication costs $300 per month and your copay is $50, the card might reduce it to $10. Just make sure your insurance is private-these cards won't work for Medicare or Medicaid patients.
Understanding your insurance plan's rules
Your insurance plan plays a huge role in how much value you get from the card. Many plans use something called a copay accumulator programa policy where the manufacturer's payment doesn't count toward your deductible or out-of-pocket maximum. This means even if the card covers $200 of your $300 copay, you still have to pay the full $300 toward your deductible. As of 2023, about 70% of commercial health plans use this type of program according to the Kaiser Family Foundation (KFF). Other plans use a copay maximizer programa policy where the manufacturer's payment counts toward your deductible or out-of-pocket maximum, which is more patient-friendly. Always ask your insurance provider: "Do you use a copay accumulator or maximizer program?" This simple question can save you thousands later.
Annual limits and tracking your benefits
Copay assistance cards usually have yearly limits. For example, many cards offer up to $8,000 in annual assistance. If your medication costs $2,000 per month, the card would cover your full copay for the first four months. After that, you'd pay the full amount unless your plan uses a maximizer program. Tracking your usage is critical. Most manufacturers provide online portals where you can see how much assistance you've used. Set a reminder to check this every month. If you're nearing the limit, contact the manufacturer's patient assistance program a month early. They might have additional support options to prevent gaps in your treatment. A common mistake is waiting until the card runs out before seeking help-this often leads to delays in getting your medication.
Alternatives when copay cards aren't an option
If you're on Medicare Part D, Medicaid, or don't have insurance, copay assistance cards won't work. Instead, consider pharmacy discount cardsthird-party cards that negotiate lower prices with pharmacies for generics or brand-name drugs. Services like GoodRx or SingleCare offer these cards. They're free, work with any pharmacy, and can save up to 80% on medications. For example, a $500 prescription might cost just $80 with a discount card. Another option is patient assistance programsdirect aid from drug manufacturers for low-income patients. These programs often require proof of income but can cover 100% of medication costs. Check if your medication manufacturer offers one-they're separate from copay cards and work for Medicare patients too.

What to do when your card runs out
When your copay card benefits end, don't panic. First, contact the manufacturer's patient assistance program immediately. Many companies have emergency support for patients who hit their annual limit. If that doesn't work, ask your doctor about switching to a generic version or a different brand that has better coverage. For example, if you're taking a specialty biologic for rheumatoid arthritis, there might be a biosimilar with lower costs. Also, explore state-specific programs. California's AB 1514 law requires insurers to count manufacturer payments toward out-of-pocket maximums, which can reduce your costs. If you're struggling financially, organizations like the Patient Access Network Foundation (PAN) offer grants for medication costs. Always act before the card runs out-waiting until the last minute can disrupt your treatment.
Frequently Asked Questions
Can I use a copay assistance card with Medicare?
No. Federal law prohibits using manufacturer copay assistance cards with Medicare Part D. Instead, look into Medicare's Extra Help program or contact your drug manufacturer for other assistance options.
What's a copay accumulator program?
A copay accumulator program is a policy where your insurance doesn't count the manufacturer's payment toward your deductible or out-of-pocket maximum. For example, if your card covers $200 of a $300 copay, you still pay the full $300 toward your deductible. This can lead to higher costs later in the year.
Do copay assistance cards work for generics?
Generally, no. These cards are designed for brand-name medications, especially specialty drugs without generic equivalents. For generics, pharmacy discount cards like GoodRx usually offer better savings.
How do I know if my insurance uses a copay accumulator?
Call your insurance provider and ask: "Do you use a copay accumulator or maximizer program?" You can also check your plan documents or ask your pharmacist during prescription pickup. Most insurers will disclose this information if asked directly.
What if I can't afford my medication after the card runs out?
Contact your doctor about switching to a lower-cost alternative. You can also apply for patient assistance programs through the manufacturer or nonprofit groups like PAN Foundation. For urgent needs, some pharmacies offer short-term discounts or payment plans-always ask.







Mayank Dobhal
February 6, 2026 AT 15:27Copay cards are a lifesaver, but accumulator programs can really screw you over.
Lakisha Sarbah
February 8, 2026 AT 09:19this is really helpful info. i didnt know about the accumulator programs. thanks for sharing. gona check my plan.
Ariel Edmisten
February 8, 2026 AT 23:56Great explanation. Copay cards are a lifesaver for many. Just remember to check if your insurance uses an accumulator program. It makes a big difference.
Niel Amstrong Stein
February 10, 2026 AT 00:12Wow, this is deep. 🤔 Copay cards are cool, but the accumulator thing is wild. Insurance doing that is like they're trying to make you pay more. Anyway, good info. 👍
Paula Sa
February 10, 2026 AT 04:44I think this is really important. Many people don't realize how accumulator programs work. It's good to know that some plans are better. Thanks for the detailed breakdown.
Mary Carroll Allen
February 10, 2026 AT 14:46OMG this is so important! I had no idea about copay accumulators. 😱 Like, if your card covers $200 but you still pay $300 towards deterent? That's insane. Gotta check my plan.
Joey Gianvincenzi
February 11, 2026 AT 14:22The information provided is of paramount importance. However, it is imperative that individuals understand the nuances of copay accumulator programs. Failure to do so may result in significant financial hardship. I must stress this point.
Ritu Singh
February 12, 2026 AT 12:17This is a critical topic. It is essential for all patients to be aware of the implications of copay accumulator programs. As a healthcare advocate, I urge everyone to verify their insurance policies. Knowledge is power.
Mark Harris
February 12, 2026 AT 19:47Whoa, this is clutch! Copay cards can save your butt, but watch out for those accumulator programs. Check your plan ASAP. You're welcome!
Savannah Edwards
February 12, 2026 AT 20:03I really appreciate this detailed breakdown.
It's so important to understand how copay assistance cards work, especially because the insurance companies have these sneaky policies like accumulator programs.
I had no idea that even though the card covers part of your copay, it doesn't count toward your deductible.
That's why it's so crucial to ask your insurer if they use a maximizer or accumulator.
For example, if you have a $300 monthly drug cost and your copay is $50, but the card covers $40, you still have to pay the full $50 towards your deductible.
This can really add up over time.
I remember when my friend was on a specialty drug and the card ran out after four months.
She didn't realize the accumulator was in place, so her deductible was still high.
It's really frustrating because you think the card is helping, but it's not really helping with the overall costs.
You have to be proactive and ask questions.
Also, for people on Medicare, there are other options like Extra Help or manufacturer assistance programs.
It's really important to know all your options.
Don't wait until you're in a bind. Reach out early.
There are organizations like PAN Foundation that can help.
This info could save someone a ton of money and stress.
I'm glad someone took the time to explain this clearly.
It's easy to get overwhelmed, but breaking it down like this makes it manageable.
Always check with your pharmacist too-they can help clarify things.
Catherine Wybourne
February 14, 2026 AT 00:31Oh, so copay cards aren't as magical as they seem? 🤦♀️ I mean, I knew insurance had tricks, but 'accumulator programs' are a whole new level of sneaky. Thanks for the heads-up-wouldn't want to get hit with a surprise deductible bill. Always good to know the fine print, right? 😏
Ashley Hutchins
February 15, 2026 AT 13:30this is why people dont read the fine print. you should have known about accumulator programs. its your fault if you get hit with high costs. dont blame the system. check your insurance details before its too late. so many people are clueless
Amit Jain
February 16, 2026 AT 17:01Nah, these copay cards are a scam. Pharma companies just want to keep you hooked. They don't care about you. Always be skeptical. There's gotta be a catch. Don't trust them. They'll screw you over eventually.
Sarah B
February 18, 2026 AT 14:07Copay cards help but you need to know the rules. Accumulator programs are bad. Check your insurance. No excuses. Do it now